
BRIDGE-ENHANCED ACL REPAIR: PRECLINICAL STUDIES
113
frequently observed after ACL injury and
reconstruction in human patients. However, the
underlying mechanism of the cartilage
protection is still not understood. The question
how collagen-platelet composites affect intra-
articular tissues is unknown but a subject of
ongoing investigation.
A collagen-platelet composite suffices as a
provisional scaffold and allows healing of an
immediately repaired ACL in the porcine
model. However, this technique was less
effective in the case of a repair performed with
a delay of two or six weeks. The reason might
be apoptosis, inflammation, or a matrix
degradation within the ACL after an injury.
To understand the reaction of the ACL to an
injury, different biological principles have been
described, as well as the intra-articular milieu,
where healing would occur. Within the
ligament, fibroblasts undergo nitric oxide-
induced and caspase 9-mediated apoptosis
early after injury. Moreover, protein fragments
increase, indicating a type I collagen breakdown
[9]. These findings suggest a degradative
environment, modulated by highly activated
matrix metalloproteinases which break down
collagen proteins. The synovial membrane, as
well as the injured ligament itself after an
injury, produces these enzymes [2, 9].
Addressing the synovial fluid milieu could
enhance the understanding or possible
counteractions of these processes and improve
the results of ACL repair [5].
To decrease the cartilage breakdown in the knee
by injecting therapeutic agents could be a
potential strategy to slow or prevent the
development of post-traumatic osteoarthritis
after an ACL injury. A scenario may include
caspase inhibition to decrease fibroblast apop
tosis or to apply antagonists of inflammatory
cytokines (e.g., interleukin1 receptor antagonist).
Also, reducing the activity of metalloproteinase
might help. Therefore, short-term intra-articular
treatment with these therapeutic agents might
influence the detrimental biological processes
that initiate ligament and cartilage degradation
after ACL injury [5, 6].
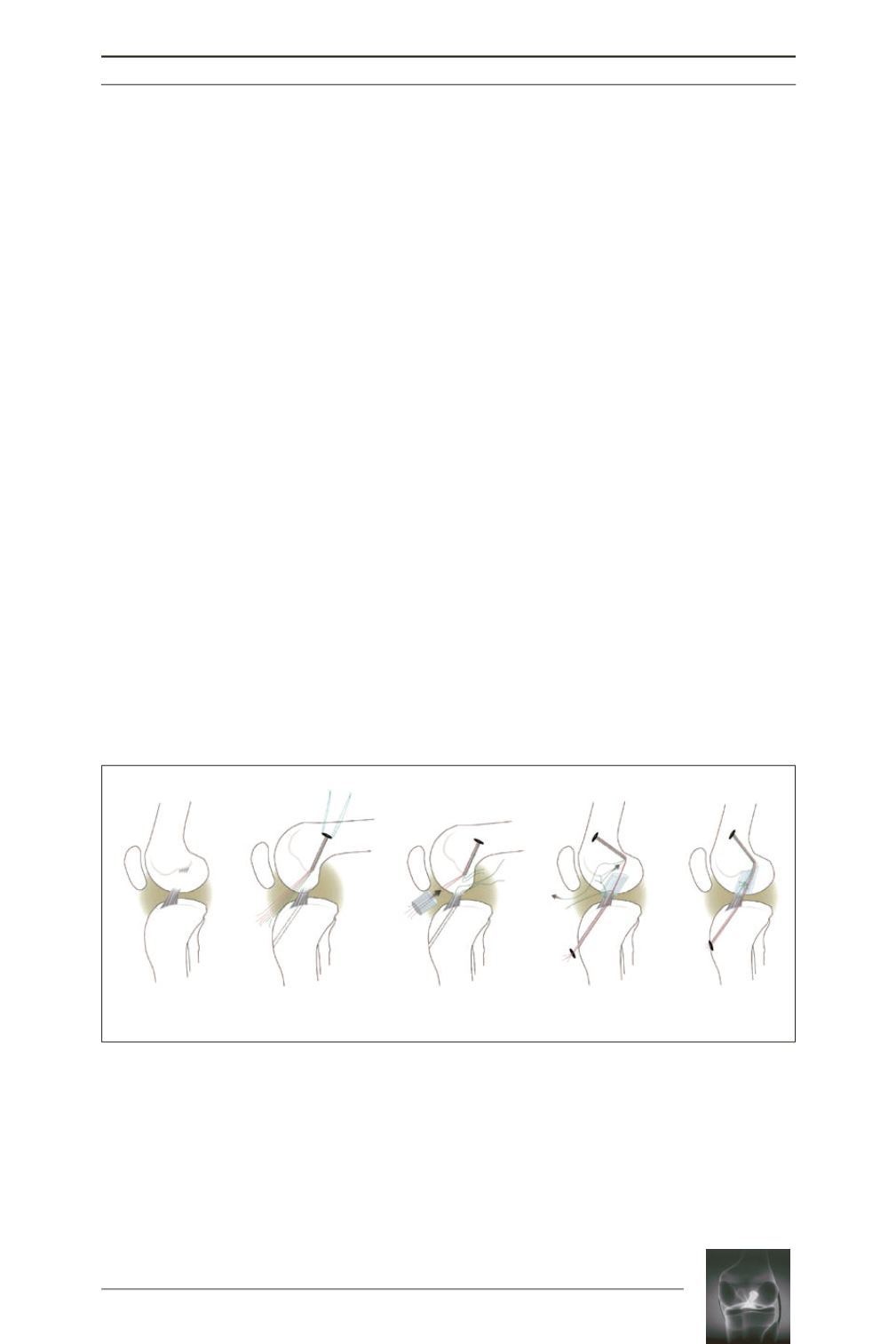
Fig. 1:
Bridge-enhanced ACL repair. (
a
) Transected ACL. (
b
) Femoral and tibial tunnels (dashed lines) and
EndoButton (Smith & Nephew Endoscopy, Andover, MA) pulled through femoral tunnel and placed on
femoral cortex. The EndoButton is loaded with 3 sutures, resulting in 6 free-ending strands (4 red and
2 green). (
c
) A Kessler suture is placed in the tibial ACL stump, and a collagen scaffold is threaded onto
4 strands (red), pushed into the notch, and saturated with 3mL of autologous blood. (
d
) The 4 suture
strands running through the scaffold (red) are passed through the tibial tunnel, whereas the remaining
suture (green) is tied to the tibial Kessler suture, using it as a pulley to reduce and stabilize the tibial ACL
stump. (
e
) The transtibial sutures (red) are tightened and tied over an extracortical button. The free ends
of the ACL suture pulley (green) are knotted to secure the reduced ACL in the collagen-platelet composite.
Reprinted with permission [10].
a
b
c
d
e











