
Sulcus deepening trochleoplasty for the treatment of recurrent patellar dislocation…
193
the patella in late degrees of knee flexion [18].
Patellar stability during early flexion is mostly
accomplished by MPFL which is tight in full
knee extension and acts as a stabilizer during
early flexion (15°-20°), brings the patella into
the trochlear grove, and in greater degrees of
flexion (>30°) is loose and the trochlea serves
as a guide for normal patellar kinematics [1].
Second, in cases of a convex trochlea, trochleo
plasty removes the sulcus prominence that the
patella needs to override during flexion and that
leads to patella dislocation off the lateral facet.
Last, trochleoplasty creates a new trochlear
groove in a more lateral position than the
dysplastic one, thus decreasing the excessive
TT-TG distance and serving as a “proximal re-
alignment procedure” [18].
The biomechanical effects of the sulcus-
deepening trochleoplasty have been studied by
Amis
et al.
who reported that the mediolateral
flattening of the anterior surface of the trochlear
facets results predominantly from an excess of
bone centrally in the groove. This forms a
supratrochlear prominence or “bump” anterior
to the shaft of the femur, which the patella has
to override when the knee starts to flex in order
to engage in the groove for the remaining
degrees of flexion. The authors showed that
“simulated” trochlear dysplasia led to
significant reduction in lateral stability and by
re-creating a deep trochlear groove with a
trochleoplasty procedure, lateral stability
increased significantly similarly to the intact
knee [26].
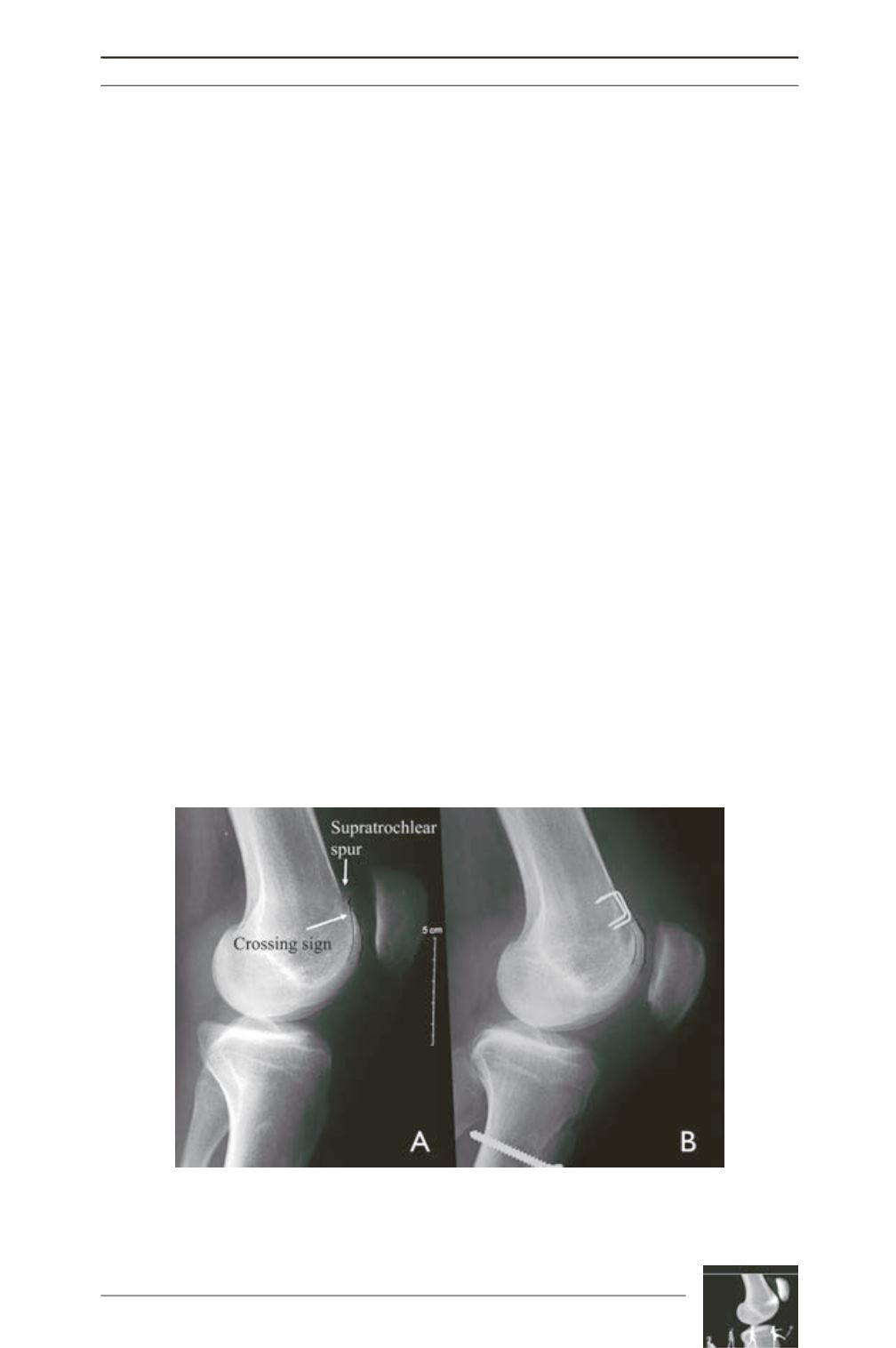
Evaluation of the results from the application
of trochleoplasty presents with certain
difficulties. There is no agreement if satisfactory
long-term results can by defined by the
correction of imaging findings (fig. 5), the
absence of pathological lateral patellar laxity,
or the restoration of the pre-operative subjective
patient’s sense of instability, pain or the absence
of apprehension [7, 8, 10]. Certainly, the latter
along with post-operative satisfaction are the
goals of any procedure for patellofemoral
instability, but authors offer different functional
scores with varying results after measuring
post-operative satisfaction in the same
population [7, 10]. Furthermore, selecting the
right candidate for trochleoplasty has been
controversial, since authors set different clinical
(pain, instability, or both) or radiological
inclusion criteria (type of dysplasia, height of
prominence) for performing such procedure [3,
Fig. 5: Example of a (A) pre-operative dysplastic trochlea type B with the
supratrochlear spur and the crossing sign, along with patella alta. (B) The
supratrochlear spur and the crossing sign disappeared after trochleoplasty and the
patella height was corrected with tuberosity osteotomy.











