
P.G. Ntagiopoulos, P. Byn, D. Dejour
188
The purpose of the present study is to record
the clinical, radiological and functional mid-
term results from the application of “Lyon’s
sulcus-deepening trochleoplasty” [18] in
patients with recurrent patellar dislocation and
underlying trochlear high-grade dysplasia.
Materials and Methods
This is a retrospective study that included
patients treated for recurrent patellar dislocation
between September 1993 to September 2006.
Inclusion criteria for the study were the
following: patients with recurrent or more than
3 documented episodes of patellar dislocation
and underlying trochlear dysplasia and
pathologic lateral patellar glide test using the
quadrant test (patella can be shifted by 3 or
more quadrants laterally by the examiner with
patient’s knee placed at full extension). Patients
with open growth plates, patellofemoral
arthritis and patellofemoral pain syndrome
with no true dislocation were excluded from
the study.
Pre-operative objective evaluation included
apprehension test, lateral patellar glide test and
patellar tracking. Subjective findings included
the presence of patellofemoral pain and/or
sense of instability. Radiological assessment
included true lateral X-rays, axial view of the
patella at 30° degrees of flexion and computed
tomography. Trochlear dysplasia was graded
and sulcus angle, lateral patellar tilt (without
quadriceps contraction), tibial tuberosity –
trochlear groove (TT-TG) distance and patellar
height (according to Caton-Deschamps index
[21]) were measured.
Patients were divided in two groups: Group A
with recurrent dislocation after previous
surgery and Group B with no surgical
antecedent. Patients were treated surgically
following an “à la carte surgery” rationale [17]
that included the identification of abnormal
anatomic factors contributing to instability and
the correction of them one by one in the same
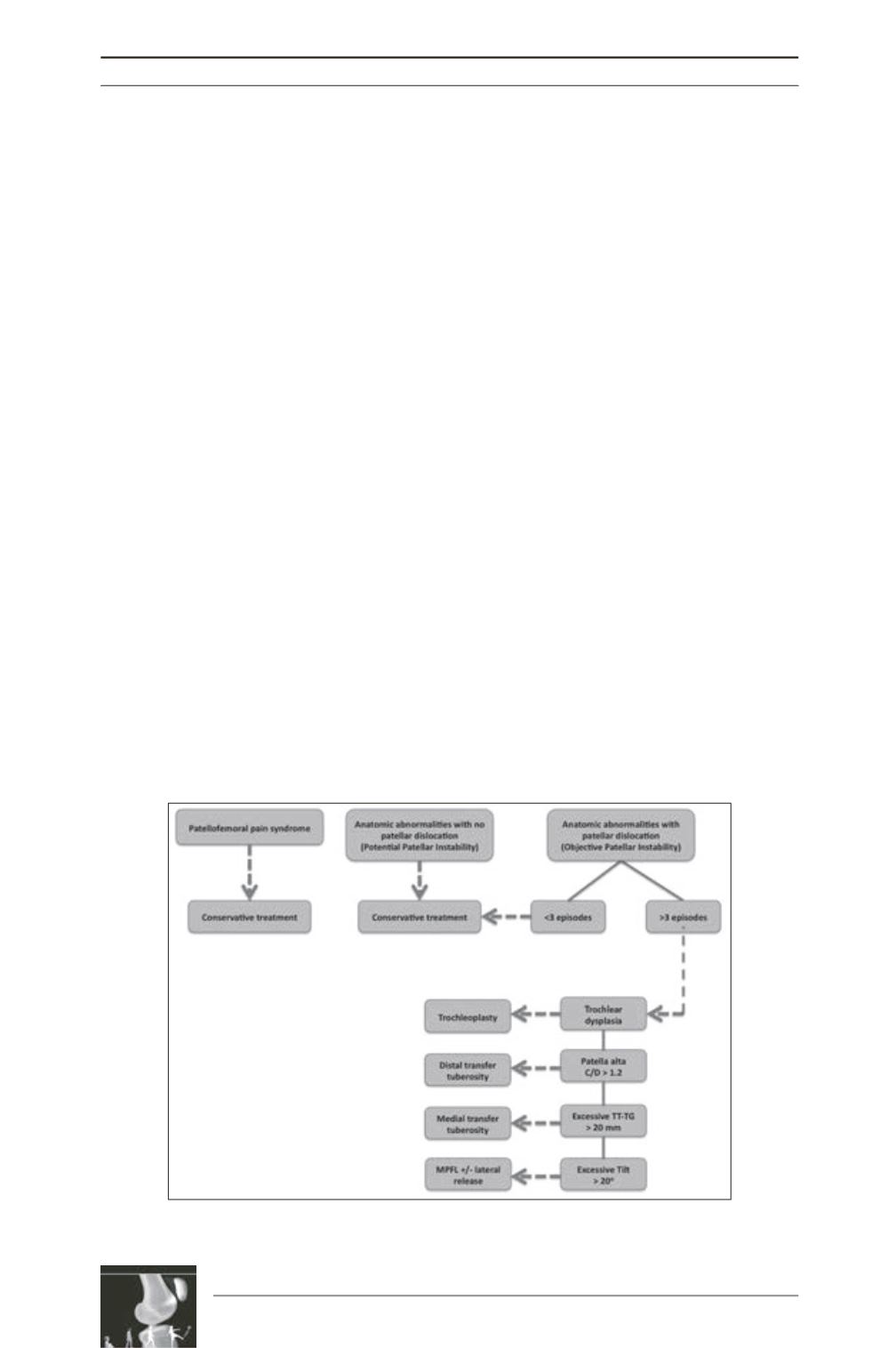
stage [2, 14, 22] (fig. 2). In all patients,
trochleoplasty was combined with medial soft-
tissue surgery, such as vastus medialis obliquus
(VMO) plasty or medial patellofemoral
ligament (MPFL) reconstruction in all knees
and, when required, with lateral soft-tissue
surgery such as lateral release or lengthening.
In patients where additional osseous etiologic
factors were recognized, a re-alignment proce
dure was added.
Fig. 2: The “à la carte surgery” algorithm that the authors followed
for the therapeutic approach of patellofemoral instability.











