
Sulcus deepening trochleoplasty for the treatment of recurrent patellar dislocation…
189
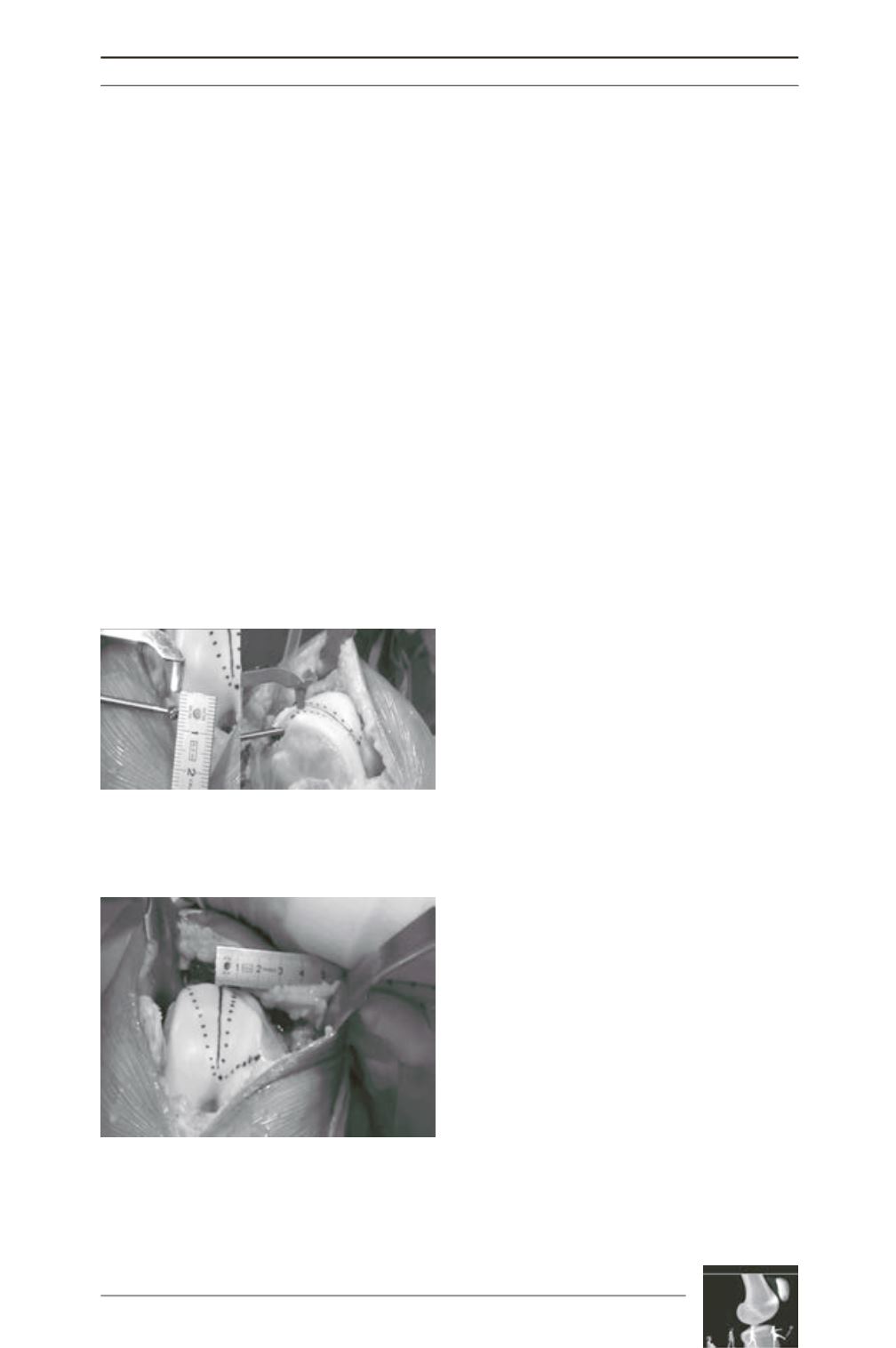
Sulcus-deepeningtrochleoplastywasperformed
with the same surgical technique in all patients
[18]. The rationale is to remove enough
subchondral bone under the trochlea (fig. 1), so
that the subsequent depression of the new
trochlear groove will be flush with the anterior
femoral cortex and the prominence will
disappear (fig. 3). The trochlea is osteotomized
with a scalpel carefully over the position of the
desired new groove, so that a normal smaller
sulcus angle is restored and the trochlear groove
is positioned in a more lateral position to
decrease the TT-TG distance (fig. 4) according
to the TT-TG value. The new trochlea is fixed
with 2 metallic staples. All patients followed
the same rehabilitation protocol described in
the relevant chapter.
Post-operative clinical evaluation was performed
at 1, 3, 6, 12 months and the last follow-up was
during May-August 2008. It included clinical
and radiological examination, IKDC score [23]
and level of activity at final follow-up. At final
evaluation, patients were also asked on their
overall satisfaction from the operation.
Statistical analysis: Differences between pre-
and post-operative mean values were compared
by the paired chi-square test. Level of statistical
significance was <0.01.
Results
Forty-nine patients were retrospectively
included. GroupAwith previous patellofemoral
surgery had 22 patients (24 knees) with prior
unsuccessful surgery for patellar instability.
Mean age was 23±5.5 years (14-33) at the time
of surgery with a female to male ratio of 1.33.
Thirty-three per cent had a positive familiar
history (first degree relative) of recurrent
patellar dislocation and 9% had bilateral
surgery. Mean follow-up was 6 years (2-8) and
no patients were lost to follow-up. Average
number of previous surgery for patellofemoral
instability was 2 per patient and included:
medialization of the tibial tuberosity,
distalization of the tibial tuberosity, soft-tissue
surgery (medial structures augmentation, lateral
structures release) and arthroscopy (Table 1).
Patients’ symptoms and clinical signs were
lateral patellar dislocation (100%), patello
femoral pain (12.5%), positive apprehension
sign (91.6%) and abnormal patellar tracking
(81%). Trochlear cartilage lesions before
trochleoplasty were: 62.4% had ICRS grade 0,
8.3% grade I, 20% grade II, 8.3% grade III, 0%
grade IV, and for the patella 45.5% grade 0, 4%
grade I, 21% grade II, 17% grade III, 12.5%
grade IV. Sulcus-deepening trochleoplasty was
combined with an additional operation in all
cases: MPFL reconstruction in 45.8% of the
cases (n=11), VMO plasty 41.6% (n=10), tibial
tuberosity distalization 20.8% (n=5), tibial
tuberosity medialization 29.1% (n=7), patellar
tendon lengthening (for previous patella infera)
8.3% (n=2), lateral release 25% [6], patellar
osteotomy 4.1% (n=1) (Table 1). Pre-operative
and post-operative radiographic findings are
Fig. 3: Subchondral bone is removed under the
trochlear without damaging the cartilage, in order to
remove the prominence and re-shape the groove.
Fig. 4: According to pre-operative TT-TG measure
ment, the new trochlear groove (solid line) can be
positioned in a more lateral position, serving as a
“proximal re-alignment procedure”.











