
J. Barth, J.C. Panisset, F. Mauris, N. Bonin, B. Sonnery-Cottet, D. Dejour
386
Results
On August 26, 2012, 94 volunteers had
participated in the survey. The mean age of
physicians was 47.5 years (30 to 65). Most of
them were French (45%) and Orthopedic
surgeons (83%). The details of answers are
listed in the following figures and tables.
The number of participants (NP) for each
question is given at the beginning to understand
the tables. For each line, the participants could
choose one answer in the various columns (C1,
C2, …, Cn). The number on each column
(NC1, NC2, …, NCn) is the number of answers.
Therefore NC1+NC2+….+NCn = NP. Column
∅
shows where most of the responses are
located. For example, if there are 4 columns
and if C1 is “never”, C2 is “sometimes”; C3 is
“often”, C4 is “always”, and
∅
= 2.5, this
means that most of the answers are located
between “sometimes” and “often”. Column G
is the mean score of subjective confidence for
each item. For example, 0% means that the
item is not relevant, whereas 100% means that
the item is highly relevant.
Discussion and
Conclusion
This was not a literature review but a general
practice analysis on an international sample of
physicians. We will give you our opinion later,
without any scientific evidence but based on our
local experience (Level 5: Expert Opinion).
The preferred imaging for early postoperative
care (3-6 months) was plain X-rays whereas
MRI was the gold standard after 6 months. On
plain X-rays, one might consider tunnel
placement, especially tibial or femoral tunnels
paced too anteriorly, fractures due to graft
harvesting such as for patellar tendon or
quadriceps tendon, but also patellofemoral
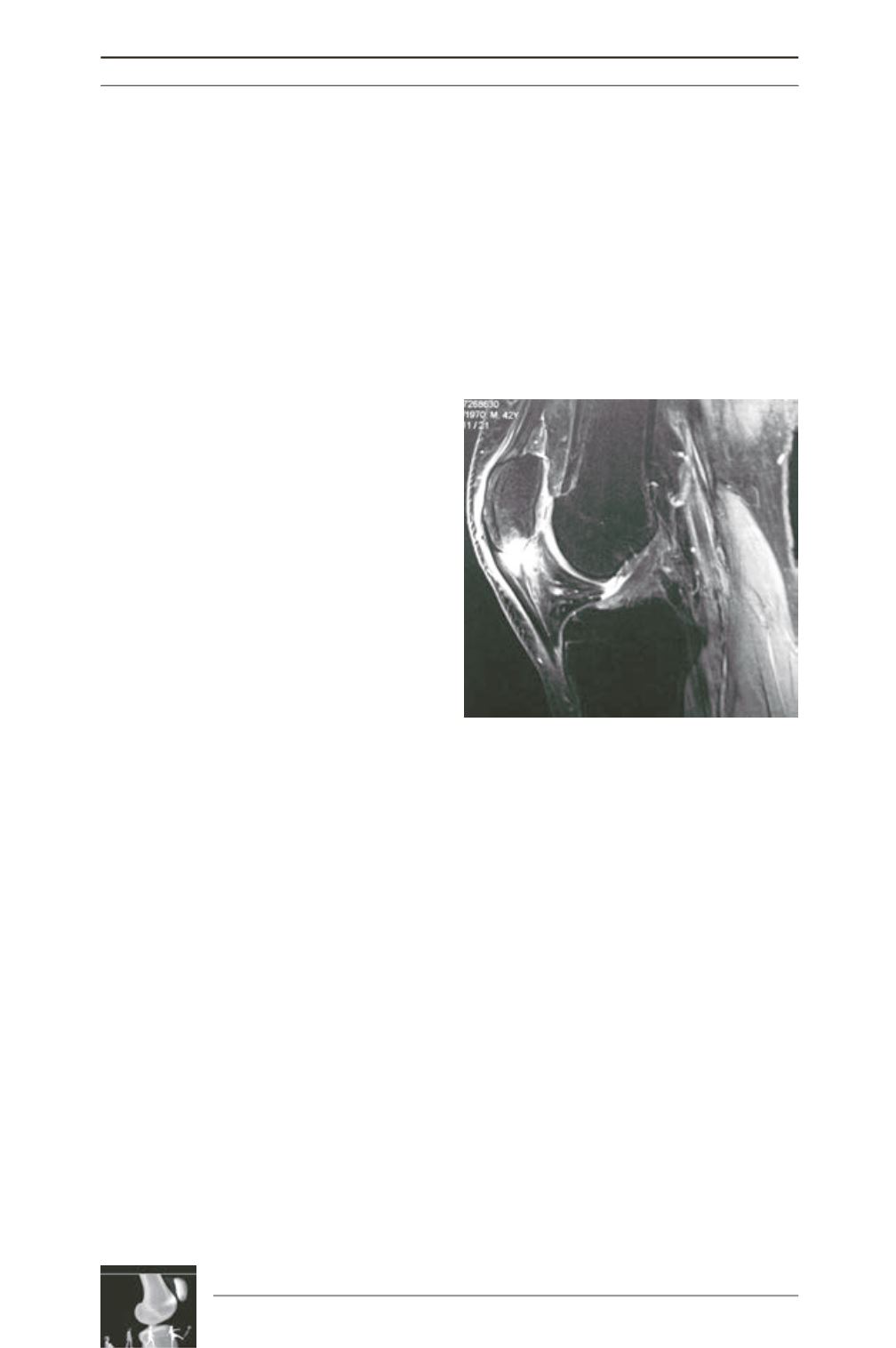
dysplasia. MRI scans are useful to screen for
Cyclops syndrome, bone bruising around
tunnels, edema in the fat pad, arthrofibrosis
around the graft, tendinitis (fig. 2), or meniscal
lesions. We agree that ultrasound is not always
contributive to understand anterior pain,
especially for intra-articular problems, even
though some peripheral disorders may be
identified with this inexpensive exam.
Examinations with an injected contrast medium
may to required in doubtful cases, such as
cartilage lesions, meniscal bucket handle
lesions, or on the physician’s special requestor
associate an injection of corticoids. Arthro-MRI
is probably the best option to avoid radiations
and it allows better evaluating soft tissues.
Isokinetic evaluation seems to become a routine
tool since only 20.5% of participants had no
access to the machine. Indeed, it is the only
way to have an objective evaluation of the
functional recovery of muscle chains (extensors
and flexors), with precise and reproducible
measures. Moreover some conditions such as
the patellofemoral syndrome may be diagnosed
by analyzing the shape of the curves.
Our physicians embraced the self-rehabilitation
protocol to treat anterior knee pain, using
cryotherapy, stretching, and cycling (67 to 79%
of reliability). These standard techniques were
also commonly prescribed by physicians, with
supervised rehabilitation by a physiotherapist.
Scar massage, deep transverse massage, and
shockwaves seem to be more controversial
(46 to 50% of reliability). However, in severe
Fig. 2: Anterior knee pain
related to patellar tendinitis.











