
Anterior Knee Pain 3 Months after acl Reconstruction: an International Survey of Practice
387
cases of tendinitis after a failed standard
treatment and within a reasonable delay (after
one year), shockwaves might be helpful but we
are currently lacking evidence.
Isokinetic rehabilitation proved to be of real
interest since it was considered reliable for
67% of our participants. We believe that this
technique improves the standard technique of
cycling by providing better feedback on the
patient’s reactions and it offers the possibility
to use eccentric strengthening programs.
Analgesics and NSAIDs were considered as
standard
for
symptomatic
treatment
(respectively 65 and 63%of reliability) whereas
corticoids, PRP, mesotherapy, conservative
podiatric management, local NSAID were
rarely believed to be effective to relieve anterior
knee pain (oscillating between 19 and 38% of
reliability). The use of cortisone injection and
visco-supplementation is more controversial
but should find a place in cases of cartilage
lesions in the patellofemoral or tibiofemoral
compartment.
We believe that the “tendinitis” should no
longer be used for all disorders related to
anterior knee pain. The physician needs to
differentiate structural or anatomical lesions
from functional problems. To do so, the first
step is to obtain objective findings such as
postoperative plain X-ray pictures to look for
patellofemoral dysplasia (N. Bonin reported
15% of dysplasia in the population of ruptured
ACLcompared to3%in the general population),
fractures, osteopenia (reflex sympathetic
dystrophy), patella bipartita, tunnel mal
positioning, type 2 Patella in the Grelsamer
classification [1] (the “big nose” that could be
a cause of tendinitis by impingement).
Furthermore, MRI should be performed to
identify the precise origin of the pain that could
be inside the patellofemoral compartment or be
an anterior projection of a femorotibial
compartment disorder. In the patellofemoral
compartment, one might look for cartilage
edema, tendinitis, Hoffa syndrome, Cyclops
syndrome, synovitis, arthrofibrosis, or bone
bruising (condyles or tibial tunnel) [2]. The
femorotibial compartments need to be screened
as well for cartilage or meniscal lesions. If no
structural lesion can be seen on the MRI and if
a neuropathic or neurological problem (such as
neuroma of infrapatellar branches of the
saphenous nerve) is excluded by the DNS4
score, functional disorders might be
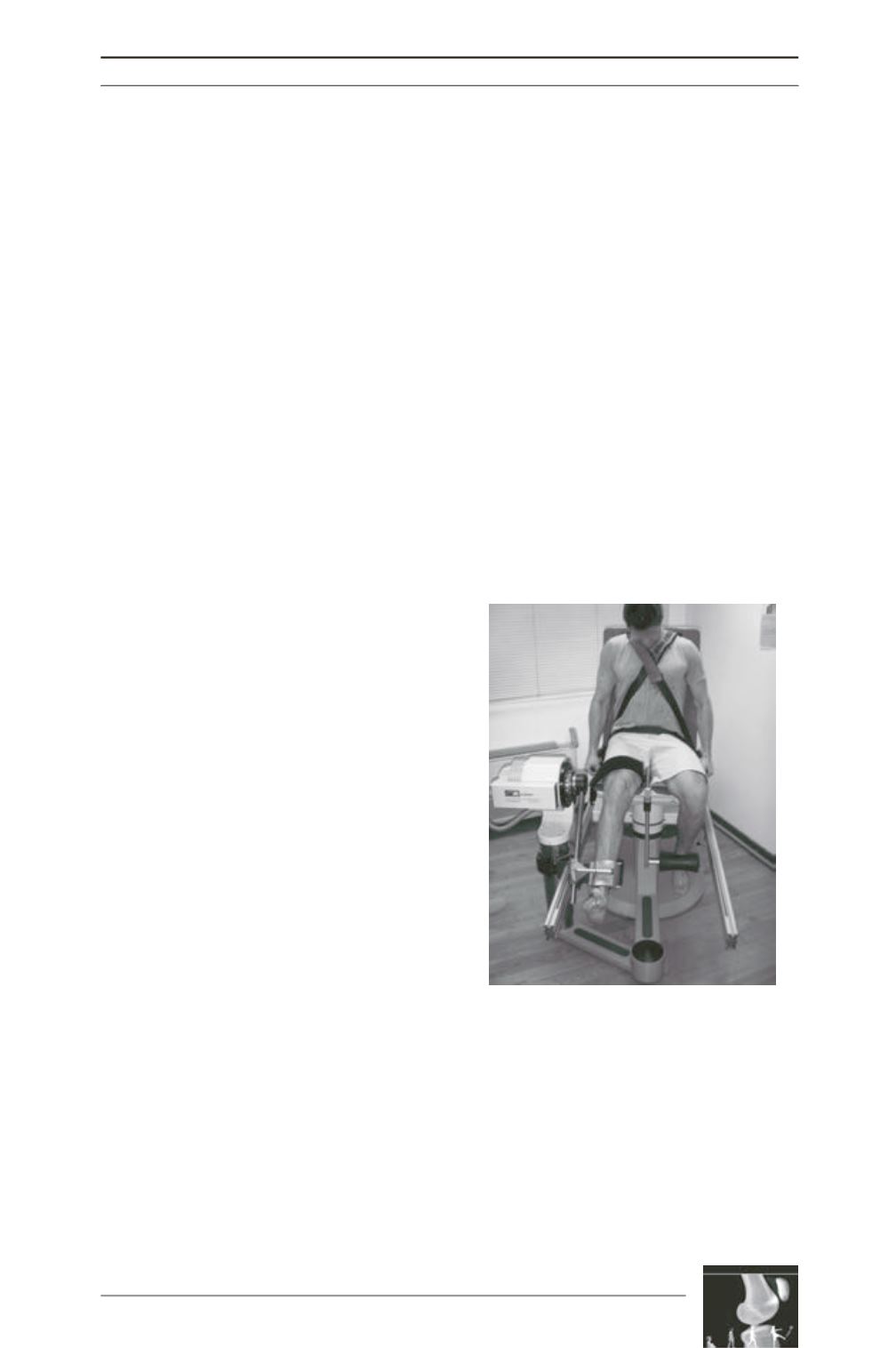
investigated with an isokinetic evaluation
(fig. 3). After 3 postoperative months, flexor
insufficiency often jeopardizes the jogging
phase. After 6 postoperative months, it is
possible to assess ratios between extensor and
flexor muscles, which need to be well balanced,
with deficits lower than 15% to avoid pain or a
new injury. Condouret showed that there was a
relationship between the level of extensor and
flexor recovery and the quality of functional
results with minimal muscle deficits close to
5% if the IKDC score was over 90 and deficits
falling to 15% in the group with IKDC score
less than 90 [3].
Once the diagnosis is accurately made, an
adapted treatment is possible in addition to
cryotherapy, NSAIDs, and painkillers. If
cycling and strengthening programs remain the
gold standard for patellofemoral pain with or
without signs of dysplasia, we learned from
E. Arendt, that core strengthening was equally
Fig. 3: Anterior knee pain due to extensor
insufficiency. Isokinetic assessment.











