
O. Courage, V. Guinet, L. Malekpour
166
Is resorting to cementless implants the solution?
We dream of biological cementing with an
integrated implant that does not alter our
resected areas. But we all have bad memories
of difficult explantations and worrisome lysis
around implants secured with screws.
But before jumping on the cementless
bandwagon with respect to these younger
patients, it would be prudent to review the
published findings.
Over 2000 studies have been published about
cementless TKA implants. Gandhi’s meta-
analysis [1] found no significant differences in
terms of outcome scores, but significantly
worse rates of loosening and radiolucent lines
with cementless implants. However, this study
is dated; the patients had more than 10 years of
follow-up and most of the implants used at that
time were not resurfaced or coated with
hydroxyapatite.
It is hard to wait for newer cementless implants
to have an equally long follow-up.
Radiostereometric analysis (RSA) can help us
fill in the gaps. RSA has the ability to detect
even 0.1mm of implant migration. The Bart
study [2] revealed how important the coating
is. Migration after 10 years was 0.79mm for
cemented implants and 1.66mm for
hydroxyapatite-coated ones, which is not a
significant difference. However, uncoated
implant migration was 2.25mm.
Julin’s study [3] of European practices found
that the use of cementless TKA varies between
countries, from 3% in Finland to 22% in
Denmark. Thus these implants have their place.
Some authors have even extended the
indications to older patients, with no particular
complications [4].
Bone regrowth was extensively studied by
Akizuhi, who concluded that hydroxyapatite
was essential to the radiolucent lines
disappearing after six months.
However, there were notable differences
between femoral and tibial components. Many
studies have shown no issues with cementless
femoral components with more than 10 years
of follow-up [6, 7, 8]. More sophisticated
RSA studies arrived at the same conclusion
[9, 10, 11].
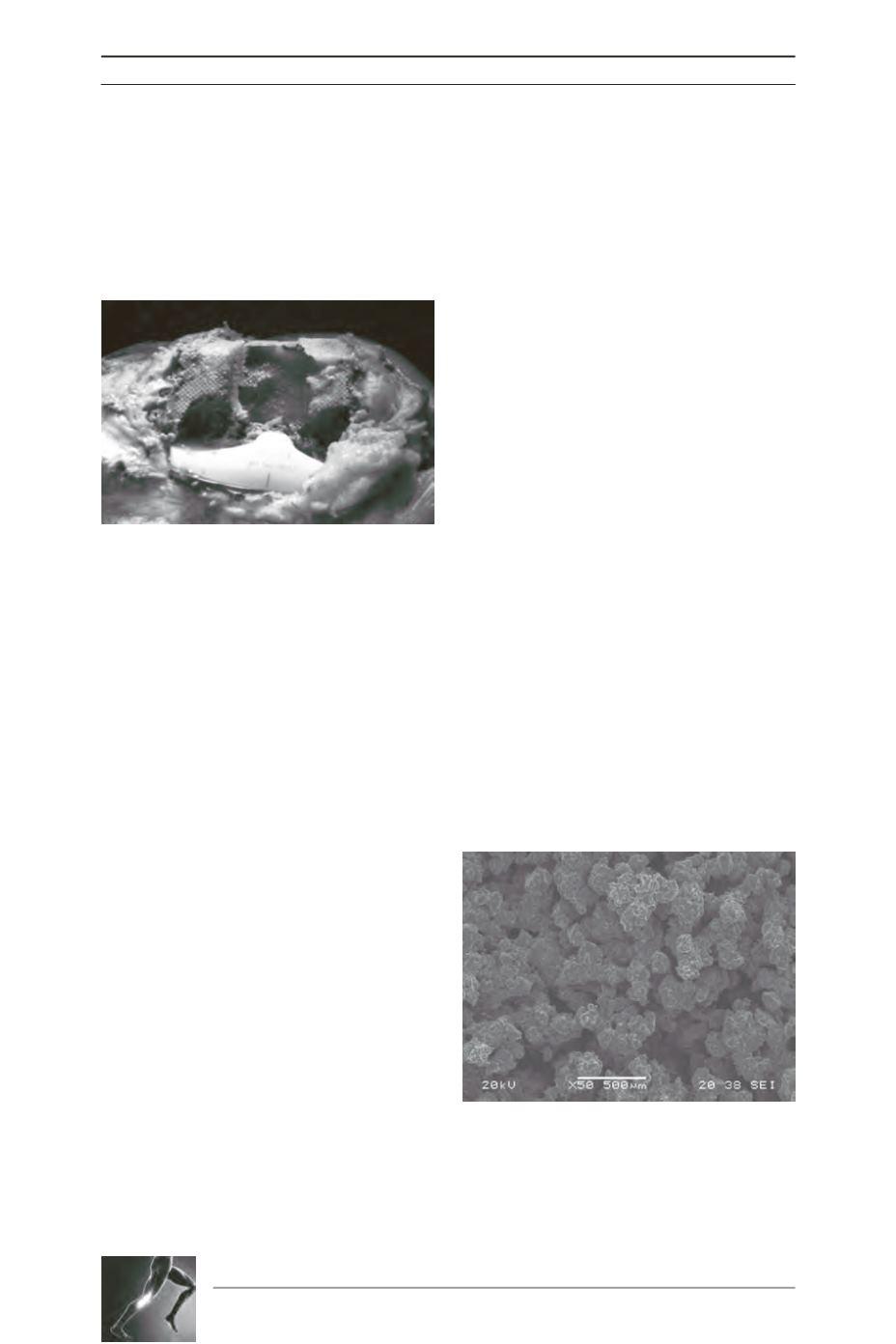
Hydroxyapatite has also been studied. Its
characteristics have an impact on the result. It
is now recommended that crystallinity greater
than 75% and a coating at least 20μm thick
should be used [12, 13]. When using a
cementless implant, the coating characteristics
are important: porosity, pore size, thickness
and material. Scanning electron microscopy
(fig. 4) reveals the main features of T
i
G
rowth
®:
porosity of 50%, pore size of 500-750μm,
1000μm thickness and titanium material.
These various coatings have been studied with
precision [14, 15, 16, 17, 18]. They are a critical
Fig. 3
Fig. 4









