
T. Ait si selmi, C. Murphy, M. Bonnin
186
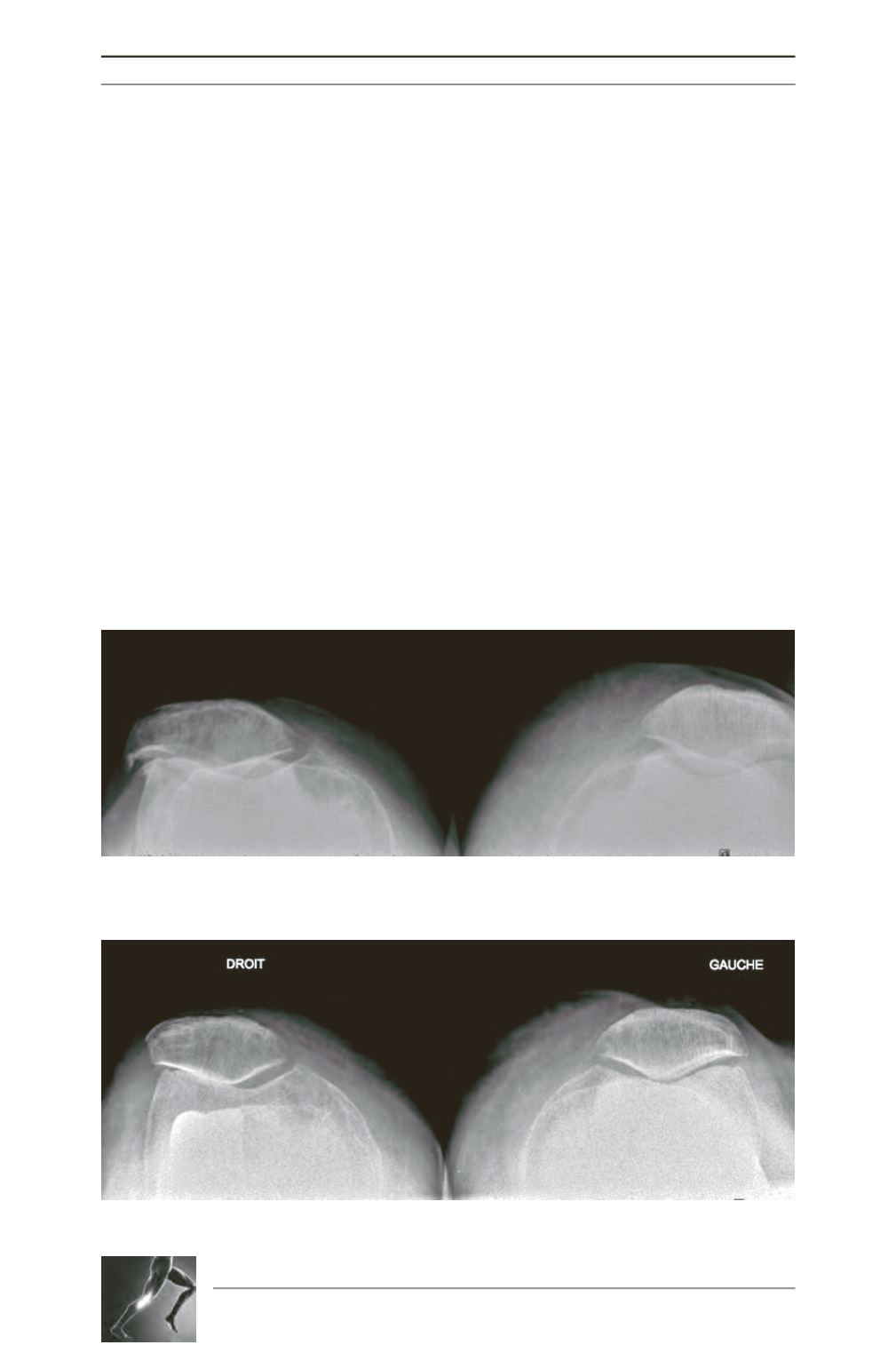
condition of this third compartment is easily
done on axial radiographs, but even established
wear in this joint is rarely considered a
contraindication to UKA (fig. 5). Beard
et al
suggest that patellar or trochlear wear seen intra-
operatively has no bearing on outcomes [4]. In
addition, complete narrowing of the lateral joint
line or the presence of large osteophytes will
influence post-operative pain. For Munk
et al.
[27], although PF wear is not a factor that
influences outcome, pre-operative lateral
patellar subluxation is associated with failure.
Patellofemoral lesions, although not a contra-
indication per se, can be managed with additio
nal procedures (such a resection of osteophytes,
a lateral facetectomy of the patella, or resection
of bony spurs on the patella) at the time of
surgery for UKA (fig. 6). Medial PF lesions,
although rarer, do not appear to affect outcome
adversely.
The Ligaments
The presence of arthritis secondary to chronic
ACL laxity is recognised by a majority of
authors as a contra-indication [9, 23]. Clinical
assessment is paramount, but in the situation
where there is already cupping of tibial condyle
things are not so clear cut. X-rays which
demonstrate significant osteophytes at the
intercondylar notch signify a damaged ACL
whose function has been affected. Translation
which fails to reduce also signifiesACL rupture.
Single leg weight-bearing lateral views are
helpful, showing posterior cupping and
spontaneous tibial translation (fig. 7).
Rarely, peripheral lesions are noted, often in a
post-traumatic setting. These are seen clinically,
further assessed on stress views, and represent
a contra-indication for surgery.
Fig. 5: Skyline view showing a patellar lateral OA and with a typical osteophyte of the right knee.
Fig. 6: Post-operative skyline view of the right knee after lateral facetectomy (preoperative view on figure 5).









