
Preoperative Planning. What I do Before a UKA
187
MRI screening
In addition to clinical examination and x-rays
imaging, MRI is very useful and is used
systematically in our service. First MRI allows
an objective measurement of cartilage in the
opposite compartment. For Yamabe
et al.
[42]
conventional imaging overestimates the degree
of cartilage damage, and retrospective MRI
assessment could have increased the number of
eligible patients from 2.3% to 58.6%. Hurst
meanwhile [16], found that abnormal pre-
operative MRI findings do not influence of the
outcome of UKA when modern radiographic
and clinical criteria are met, suggesting that
lesions on MRI might be over-estimated. The
MRI allows as well the screening of potential
meniscal lesions of the other compartment
which is missed on standard screening [26].
Clinical examination and radiological assess
ment of the PFJ are significantly improved
while combined with the MRI according to
Waldstein [41].
Assessment of the ACL ligament is useful.
Hill [14] cites a complete ACL rupture rate of
22% among the cohort of arthritic knees
examined. Nevertheless, the macroscopic
appearance can be balanced by the histological
assessment [39].
Arthritis secondary to chronic laxity must be
differentiated from an arthritis that is caused by
progressive ACL attrition or cysts due to notch
intrusion and collagen degeneration (fig. 8-10).
For these cases, no spontaneous tibial
translation is seen and ligamentous lesions are
often incomplete as seen on the MRI. In our
experience, MRI correlates well with the intra-
operative macroscopic appearance once the
notch osteophytes have been resected (fig. 11
& 12). In this particular context, the indication
for the Unicondylar prosthesis is acceptable.
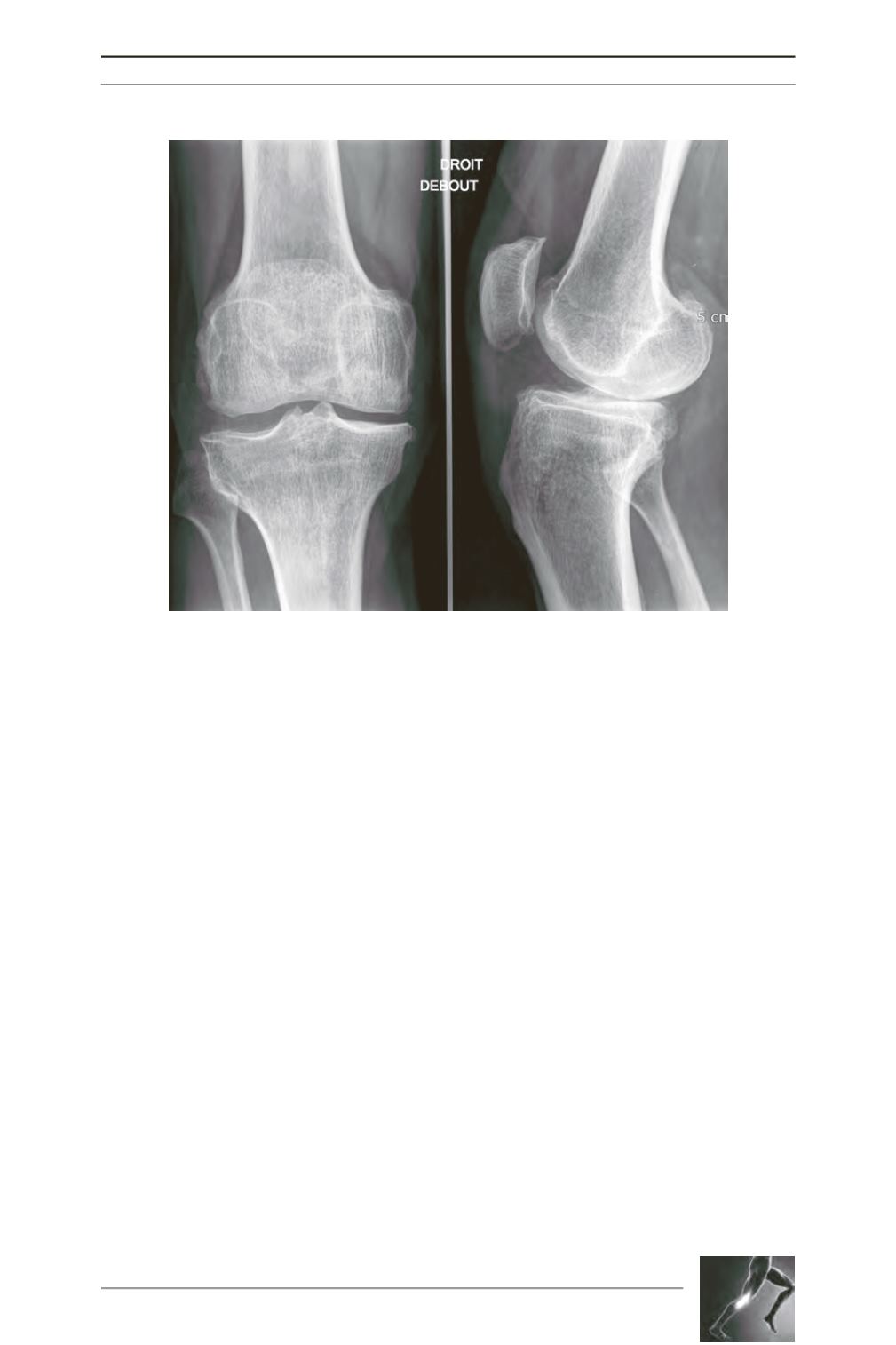
Fig. 7: Medial OA resulting from previous anterior cruciate ligament rupture with a
major spontaneous anterior tibial translation on lateral weight bearing view.









