
Bicruciate-retaining TKA: A Concept Worth Exploring
99
We investigated stiffness by splitting each
cohort in two groups, stiff knees and flexible
knees. A knee was considered stiff if it lost
10 degrees of flexion or more at the last follow-
up compared to pre-operative flexion; knees
with a flexion contracture of 5 degrees or more
at the last follow-up were also labelled as stiff,
no matter if a flexion contracture was noted
before surgery (Table 3). Using these criteria,
61% of the bicruciate-retaining TKA were stiff
(three because of a knee flexion contracture, 44
because of decreased flexion, and 14 because
of both); 35% of the posterior-stabilized knees
were stiff (seven because of a knee flexion
contracture, 27 because of decreased flexion,
and one because of both). An interesting finding
is that, in the two cohorts, stiff knees had
significantly more flexion before surgery than
flexible knees, but gained less flexion during
surgery, and lost more flexion during the post-
operative period.
So far we failed to explain why some knees
stiffened and others didn’t, although we
analyzed numerous factors including the
thickness and the alignment of bone cuts,
implant size, and ligament releases. However,
we noted that bicruciate-retained knees, either
stiff or flexible, lost more flexion than the
posterior-stabilized knees during the post-
operative period. Considering this, plus the fact
that knee stiffening was almost twice as likely
to occur with bicruciate-retaining TKA as with
posterior-stabilized TKA, it seems obvious that
the cruciate ligaments play a role. Plausible
mechanisms
include
technical
errors,
intercondylar fibrosis, and/or nociceptive
feedback from the cruciate ligaments. Patient
factors are also probably involved: indeed,
most patients of the reported cohorts that had a
TKA performed in both of their knees had a
symmetrical outcome regarding knee stiffness
(80% of 2C knees and 83% of PS knees). Our
current hypothesis is that minor technical errors
are common during performance of any type of
TKA, but that the knee is less forgiving for
them when the cruciate ligaments are retained.
The reasons for this still need to be clarified.
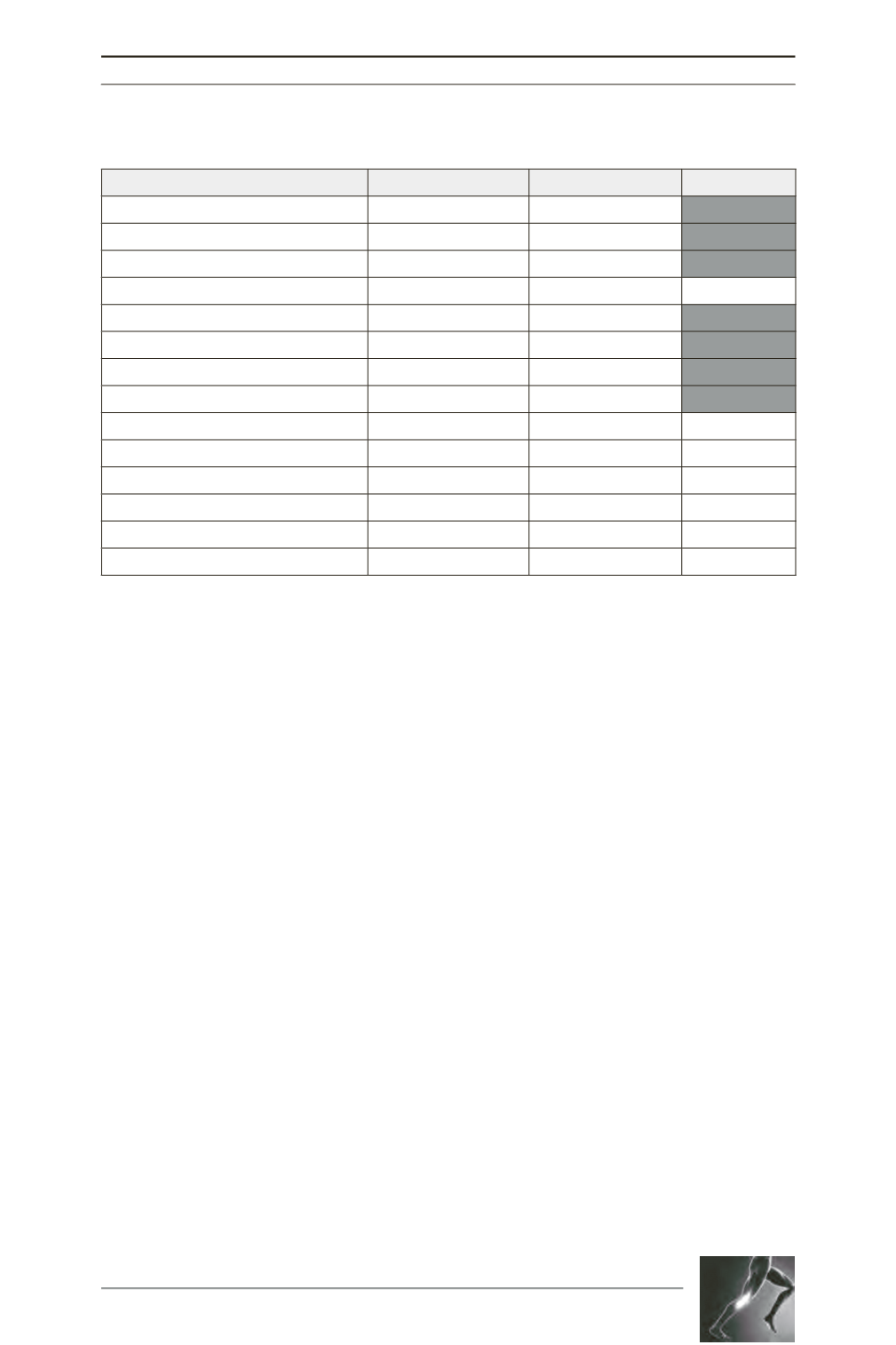
Table 2: Post-operative data for Bicruciate-retaining (2C) and Posterior-stabilized (PS) TKA cohorts.
2C
PS
p value
Follow-up length (months; range)
18 (5-50)
38 (13-71)
<0,001
Tourniquet time (minutes; range)
53 (32-112)
58 (36-113)
0,003
Patellar resurfacing (%)
18
85
<0,001
Medial HKA angle (range)
179,3 (171,8-185,8) 179,1 (171,9-187,5)
0,725
Knee flexion contracture (range)
1,5 (0-15)
0,7 (0-15)
0,034
Flexion at end of surgery (range)
132 (110-140)
127 (80-140)
<0,001
Flexion at last follow-up (range)
118 (80-150)
124 (60-150)
0,006
KS Knee Score
83,9
89,2
0,026
KS Function Score
75,1
75,6
0,874
KOOS - Pain
72,9
75,9
0,413
KOOS - Symptom
68,8
75,3
0,400
KOOS - Activities of daily life
74,9
75,4
0,894
KOOS - Sporting activities
39,2
42,1
0,564
KOOS - Quality of life
61,1
69,0
0,075









