
E.A. Arendt
120
The Lyonnais team further described a surgical
algorithm to treat patella instability by
correcting each anatomical (radiographic
imaging) abnormality. Excessive lateral patella
tilt was treated with a lateral retinacular release,
and a “VMO plasty”.
Several seminal articles describe lateral patella
tilt as an injury variable in need of surgical
correction, describing lateral patella tilt as an
imaging feature without a physical exam
association [7, 8].
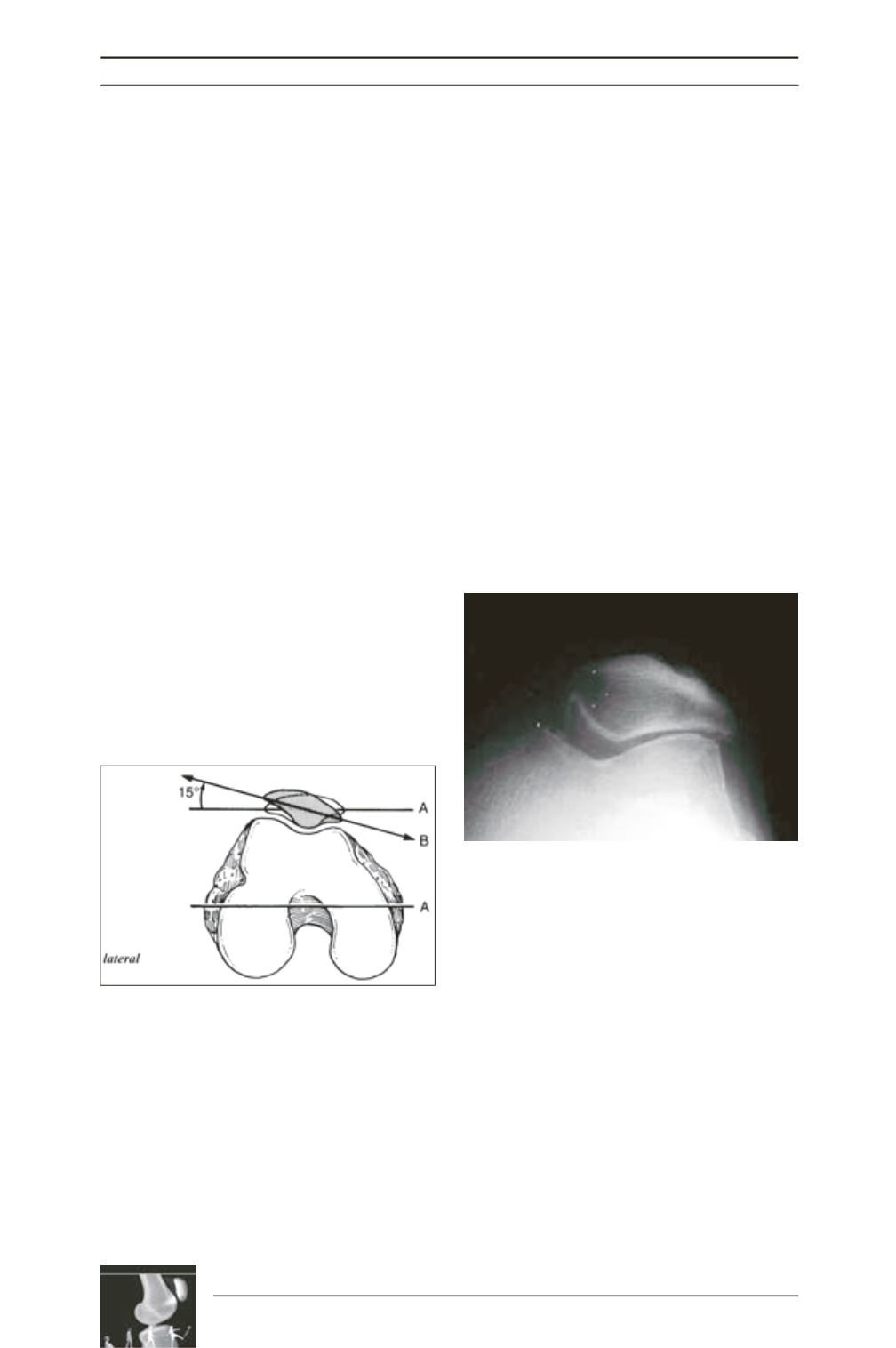
The reader is left with the assumption that the
imaging sign of excessive lateral patella tilt is
associated with tight lateral structures that
presumably needed to be lengthened or
released. Although patella tilt is difficult to
define objectively by physical exam, it is
recognized that lateral patella tilt is associated
with a decrease in medial patella translation
and negative medial patella tilt test (the inability
to bring the lateral board of the patella past the
level of the horizon) (fig. 1). When you associa
te excessive lateral patellae tilt on X-ray with a
physical exam sign of lateral tightness, this
represents patella tilt that may need to be
surgically corrected.
A critical aspect of patella tilt analysis is that
excessive lateral patella tilt may represent
lateral tightness, but it always represents some
degree of medial retinacular laxity. This is
particularly important when viewing an acute
image; one nearly always sees excessive lateral
patella tilt and a large hemarthrosis due to the
associatedtraumaofanacutepatelladislocation.
Therefore, measurement of lateral patella tilt
can be grossly over-estimated on MR, CT, or
axial radiograph when it is associated with a
large degree of knee swelling as is typical in
the acute injury phase.
Lateral patella tilt can also be mis-leading when
it is associated with loss of cartilage in the lateral
patellofemoral joint. Laurin
et al.
[9], describe
lateral patella tilt as being due to cartilage loss
from the lateral trochlea and lateral patella facet,
not tightness of the lateral retinaculum. Indeed,
we often see a “pseudo tilt” associated with
patellofemoral arthrosis, where the lateral tilt of
the patella is due to loss of cartilage in the lateral
patellofemoral joint space [10] (fig. 2), rather
than lateral patella tilt being obligated by one’s
own innate morphologic anatomy.
Noting the concerns of mis-interpreting patella
tilt
as always associated with “too tight”
lateral soft tissues structures
, it is noted that
the degree of lateral patella tilt has been shown
to have a direct relationship to the degree of
trochlear dysplasia (i.e.), high grade trochlear
dysplasia is associated with greater patella tilt
[11].Forstudentsofpatellofemoralmorphology,
the lateral soft tissue structures offer the most
challenging and diverse soft tissue dilemmas in
dysplastic patellofemoral joints.
Fig. 1: Medial Patella Tilt Test
Fig. 2 : Patella tilt due to loss of cartilage in the
lateral PF compartment (Iwano Type 3 classification
of PF Arthritis).











