
P.B. Schoettle
126
Although most of the actual surgical techniques
utilize a free tendon graft to reconstruct the
MPFL as the only method for anatomic double
bundle graft fixation, an all aperture fixation
has not yet been described.
Recent studies have described an anatomical
double bundle reconstruction, using an aperture
fixation at the femoral insertion [6, 8], while
the patellar fixation remains relatively indirect
resulting in the eventual risk of post-operative
micromotion and subsequent loosening.
Patellar graft fixation has been described with
either an anchor system, attaching the graft into
a bony rim, [6] or by tying the attached graft
sutures to each other at the lateral patellar edge
[8]; however, this method may potentially
result in graft slippage by degloving [7].
Until today, only one technique described
anatomical patellar fixation by looping graft
through bone tunnels without any additional
fixation device [9]. This technique appears to
produce stable fixation at the patella. However,
in soft bone, a widening of the tunnel could
occur in the long-term; moreover, in patients
with a short gracilis graft, the tendon length
may not be long enough to reach the anatomical
femoral insertion.
The double bundle technique described here
offers an aperture fixation at the patella and the
femur, providing a high initial stability on both
insertions, resulting in improved bony in
growth, and consequently, an earlier return
tofull range of motion.
Surgical technique
Harvesting and preparing of the
gracilis tendon
After completion of the arthroscopy, a 2cm
long oblique incision is performed at the pes
anserinus. After incising the sartorius
aponeurosis, the gracilis tendon is harvested
and used as an autograft. The load to failure
force of the Gracilis graft – even as a single
bundle-exceeds the failure to load of the MPFL
(208N). [3] The usable part of the tendon
should be at least 18cm long. After harvesting
the tendon with the stripper and removing the
muscle tissue, the doubled tendon diameter is
determined and both ends are whipstitched
with an absorbable braided suture over a length
of 15mm.
Preparing the soft tissue layer
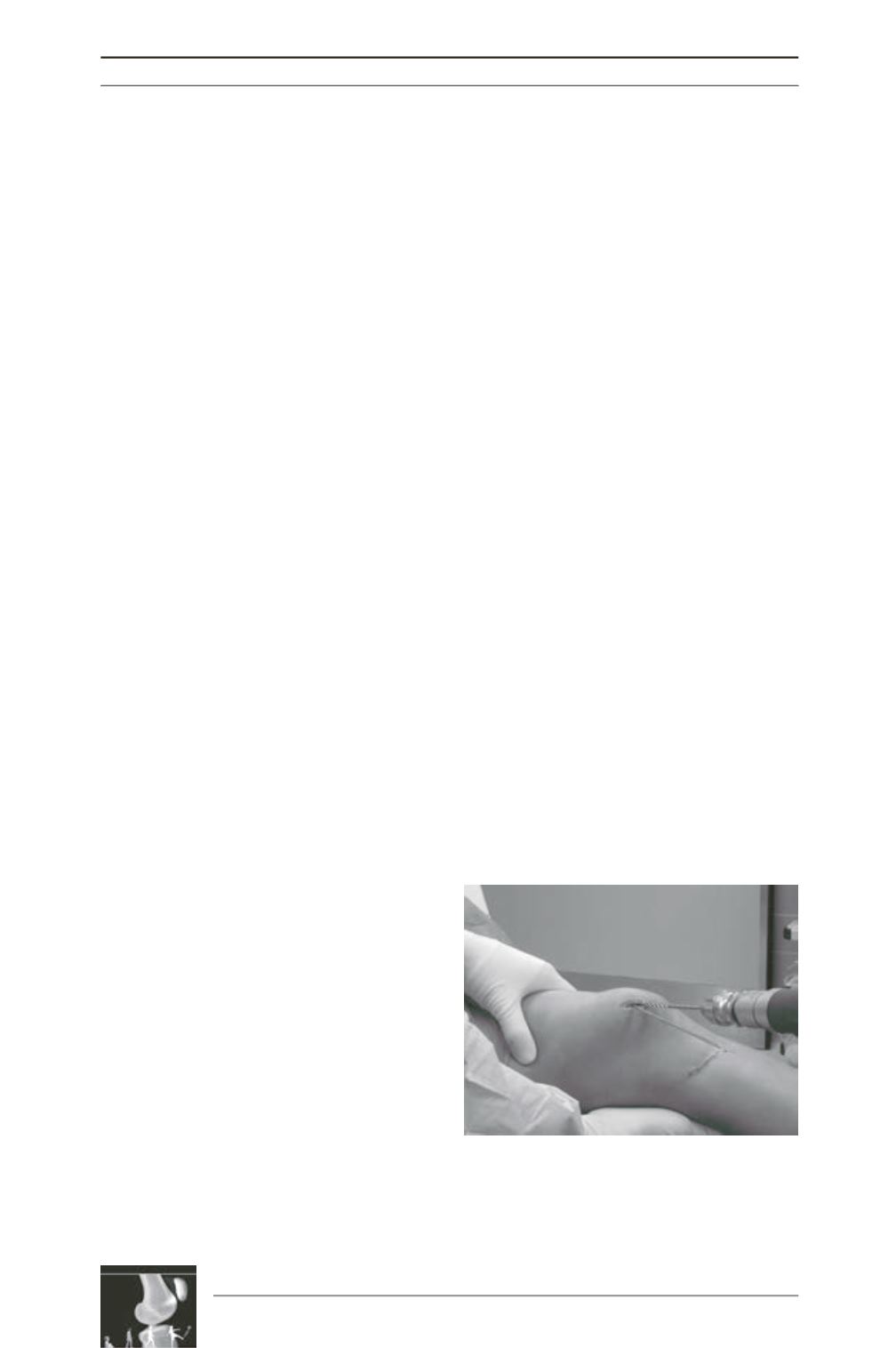
A 2cm skin incision is performed from the
superomedial corner to the end of the medial
margin of the patella, where the patellar MPFL
insertion is located [4, 10] (fig. 1). As the MPFL
is situated central to the Vastus medialis
obliquus (VMO) in the second layer of the
medial patellofemoral complex [10], the central
part of the VMO is identified and a scissor is
brought along to the medial femoral epicondyle
in between the VMO and the joint capsule,
cautiously avoiding any injury to the joint.
After the opened scissors are removed, a right
angle clamp is brought into the separated layer
and the tip is directed towards the skin in the
area of the adductor tubercle, where the femoral
MPFL insertion is located. Then a small
longitudinal skin incision is performed over the
tip in 30° knee flexion, the position wherethe
graft will be finally fixed. Finally, in preparation
for passing the final graft, a suture loop is
inserted in between the second and the third
layer using the right angle clamp.
Fig. 1: After the anatomical landmarks of the patella
are marked, a 2cm incision from the supermedial
corner of the patella to the medial margin is
performed and two 4.0mm holes are drilled for the
MPFL insertion.











