
N. Jan, P. Chambat, J.-M. Fayard
106
At the time of index procedure, the mean age
was 56 (range 38.8-67.1) years. HTVO con
cerned 8 left knees and 23 right knees. Seven
patients had no previous surgery. Varying
degrees of lateral meniscectomies were
performed in 23 patients (24 knees) before the
index procedure. Among these patients, one
has had also a distalization of the tibial tubercle
in the same procedure. In different procedures,
four patients have had varying degrees of
medial meniscectomy and one patient under
went loose-body removal under arthroscopy.
Eighteen lateral meniscectomies, four medial
meniscectomies, one loose-body removal and
five notchplasties were associated to the HTVO.
“T” plate (Tornier©) was used in 24 HTVO
and C-plate (Otis SBM©) in 7 HTVO after
2007. No bone graft was required.
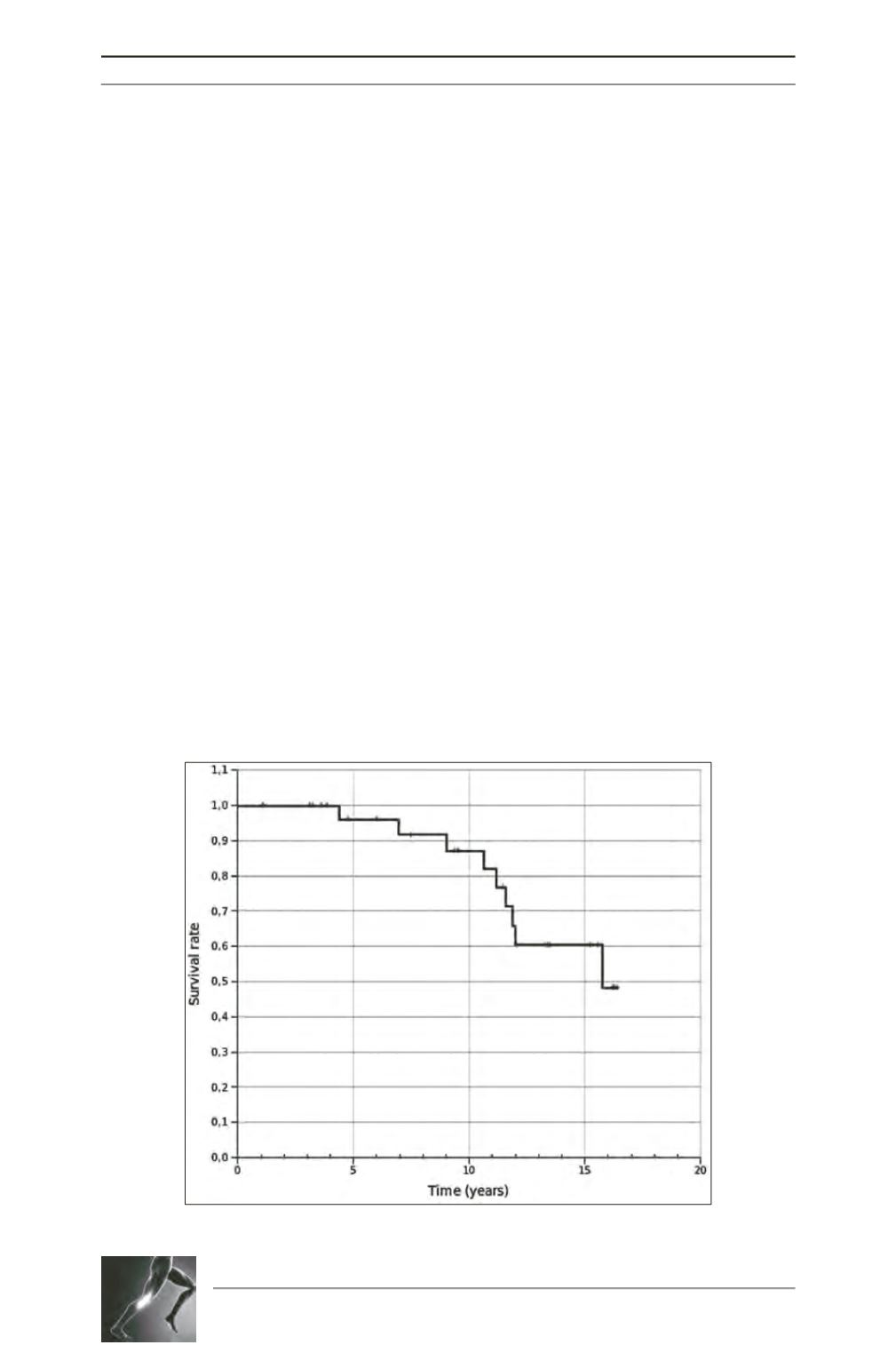
Survivorship analysis
Three patients were lost to follow-up. Revision
to total knee arthroplasty was performed at the
mean time of 10.3 years (range 4.4-15.3) in
9 patients.
In a best-case scenario, with knee replacement
as the end-point the cumulative survival rate of
the HTVO was 96% (95% CI 0.92 to 1.00) at
5 years, 87% (95% CI 0.80 to 0.94) at 10 years,
and 60% (95% CI 0.47 to 0.74) at 15 years
(fig. 2).
At the last follow-up, 23 patients were pain
relieved and declared they have improved their
activity level. Unsatisfied patients (4 cases),
patients lost to follow-up (3 cases), patients
with/or waiting for knee replacement (11 cases)
were considered as failure. In a worst-case
scenario, with failure as the end-point, the
cumulative survival rate of the HTVO was
87% (95% CI 0.80 to 0.93 at 5 years, 71%
(95% CI 0.62 to 0.80) at 10 years and 41%
(95% CI 0.30 to 0.52) at 15 years.
Clinical outcomes
At final follow-up, 13 patients could not be
included for clinical evauation: one refused,
9 patients underwent knee replacements and
3 were lost to follow up. Finally, 17 patients
(18 knees) were available for complete clinical
Fig. 2 : Survivorship analysis : best-case scenario









