
T. Ait Si Selmi, D. Shepherd, M.Bonnin
80
The 180° traditional
alignment and
balancing
Historically the proposed aim for coronal
alignment, as measured by the mechanical
femorotibial angle (MFT angle), has been
within ±3° of 0 degrees, and the longevity of
TKR has been traditionally associated with
neutral or slightly valgus coronal alignment
[20-23]. Studies have demonstrated improved
functional outcomes with coronal alignment
within 3 degrees of neutral [24, 25]. Achieving
a mechanical alignment of 0° in the coronal
plane requires the placement of the femoral and
tibial components perpendicular to the femoral
and tibial mechanical axes respectively. In the
case of the femur themechanical and anatomical
axes are not coincident and form the femoral
mechanical anatomical (FMA) angle. As such a
distal valgus cut is made with respect to the
anatomical axis, which should be equal to the
FMA angle. Generally during conventional
TKA with standard instrumentation most
surgeons use the same fixed distal valgus
resection angle (4°-7°) for all their patients,
although variable jigs are available.
This goal of alignment also has consequences
on balancing flexion and extension gaps notably
at the femoral end [26]. Balancing the knee can
be performed by utilizing measured resection
techniques and setting the posterior joint line
perpendicular to the anteroposterior axis of the
trochleargroove,paralleltothetransepicondylar
axis, externally rotated 3° with respect to the
posterior condylar axis or parallel to the tibial
resection in 90° of flexion with the use of gap-
balancing technique aligned internal-external
rotation of the femoral component.
With measured resection techniques there is a
wide range of femoral rotation, instability and
femoral condylar lift off during flexion to 90
degrees [27, 28]. Gap balancing produces more
accurate gap symmetry and minimal instability
but can raise the joint line [29], and is accurate
for gap balancing at 0 and 90 degrees but not
necessarily in mid flexion [30]. Patients who
perceive these changes in stability, limb
alignment, and joint level alignment may be
dissatisfied. The more accurate gap symmetry
of gap balancing does not produce better
functional outcomes in cruciate retaining or
posterior stabilized prostheses [29, 31].
Fundamentally the current knee prostheses are
designed with the concept that the bone cuts
and the ligaments are balanced in order to
modify the knee so as to fit the prosthesis to the
knee along these alignment principles of 0
degrees and working with a ‘square gap’.
Consequently, any intraoperative change in any
one of factor of rotation, flexion, oversizing or
balancing of components ultimately has
consequences and compromises on the other
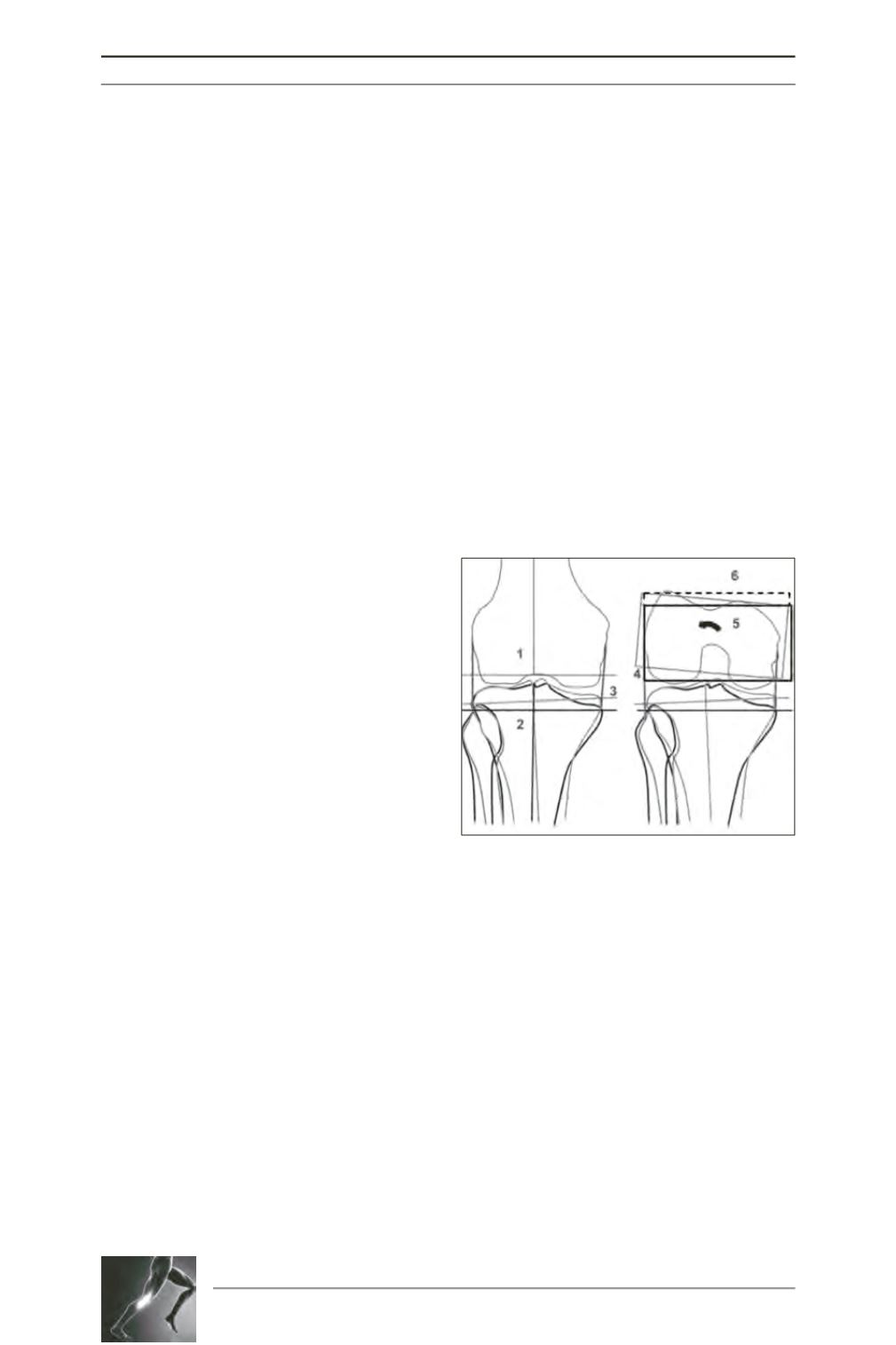
parameters (fig. 1).
Naturalalignment and
balancing
The dogma of a target of an alignment of 180°
crossing the prosthetic joint line perpendicularly
Fig. 1: Cascade of events resulting of traditional
realignment in a typical varus knee. 1) The femoral
perpendicular asymmetrical cut. 2) Tibial
perpendicular asymmetrical cut. 3) MCL release to
compensate extra-articular tibial deformity, thus
changing the joint line level. 4) Grey rectangle
underlying the posterior reference alignment,
leaving an asymmetrical posterior gap. 5) Black
rectangle showing external rotation where flexion
gap balancing option is selected. 6) Broken line:
increase of AP dimension as result of rotation with
subsequent ML increase.









