
W.B. Leadbetter
282
Maquet introduced controversy with his
anterorization tibial tubercle osteotomy for
knee arthritis [13]. Fulkerson improved upon
these concepts with his anteromedialization
tibial tubercle osteotomy (AMZ) [14].
However, despite Radin’s hopes, there was a
growing number of patients who failed to
achieve relief from the available operative
solutions. Total knee arthroplasty was in it’s
infancy and was not considered an option for
the arthritically disabled, often younger (age
less than 50 years old) patient. And so,
beginning in 1974, Blazina launched the
modern age of patellofemoral arthroplasty with
the Richard I and II prostheses. The average
patient age in his series was 39 years (range,
19- 81) [15]. At the same time in France, Cartier
began his series using the both the Richards II
and later the Richards III patellofemoral
prosthesis. As a salvage procedure, these early
experiences were encouraging. In 2005, he
would report on his experience with 70 patients,
average age 60 years (range, 36-81). There was
a prosthetic survivorship of seventy-five
percent at average follow-up of 10 years [16].
Yet, during this period prosthetic replacement
of the patellofemoral joint remained the
unpopular step child of total knee arthroplasty
primarily because of reported high revision
rates due to design deficiencies and difficult
patient selection with regard to risk of
tibiofemoral joint arthritic progression.
We will arbitrarily close this renaissance period
with two developments. The first is the
diagnosis, classification, and treatment impli
cations of trochlear dysplasia. First described
by Ficat and later refined by Henri Dejour,
Phillipe Neyret, and David Dejour, the
recognition of trochlear dyplasia proved to
have significant implications for both the
successful long term outcome and prosthetic
evolution of patellofemoral prosthetic design
[17, 18]. Argenson called attention to the
presence of trochlear dyplasia as a key factor in
predicting the success of patellofemoral
arthroplasty with respect to progressive
tibiofemoral joint involvement. It was theorized
that because this mechanical cause of premature
patellofemoral degeneration seemed indepen
dent of more genetically predisposed tricom
partment arthritis, patellofemoral dysplasia
would tend to be a marker for the selection of
thesocalledisolatedpatellofemoralarthroplasty
case [19]. Others would agree [20, 21]. The
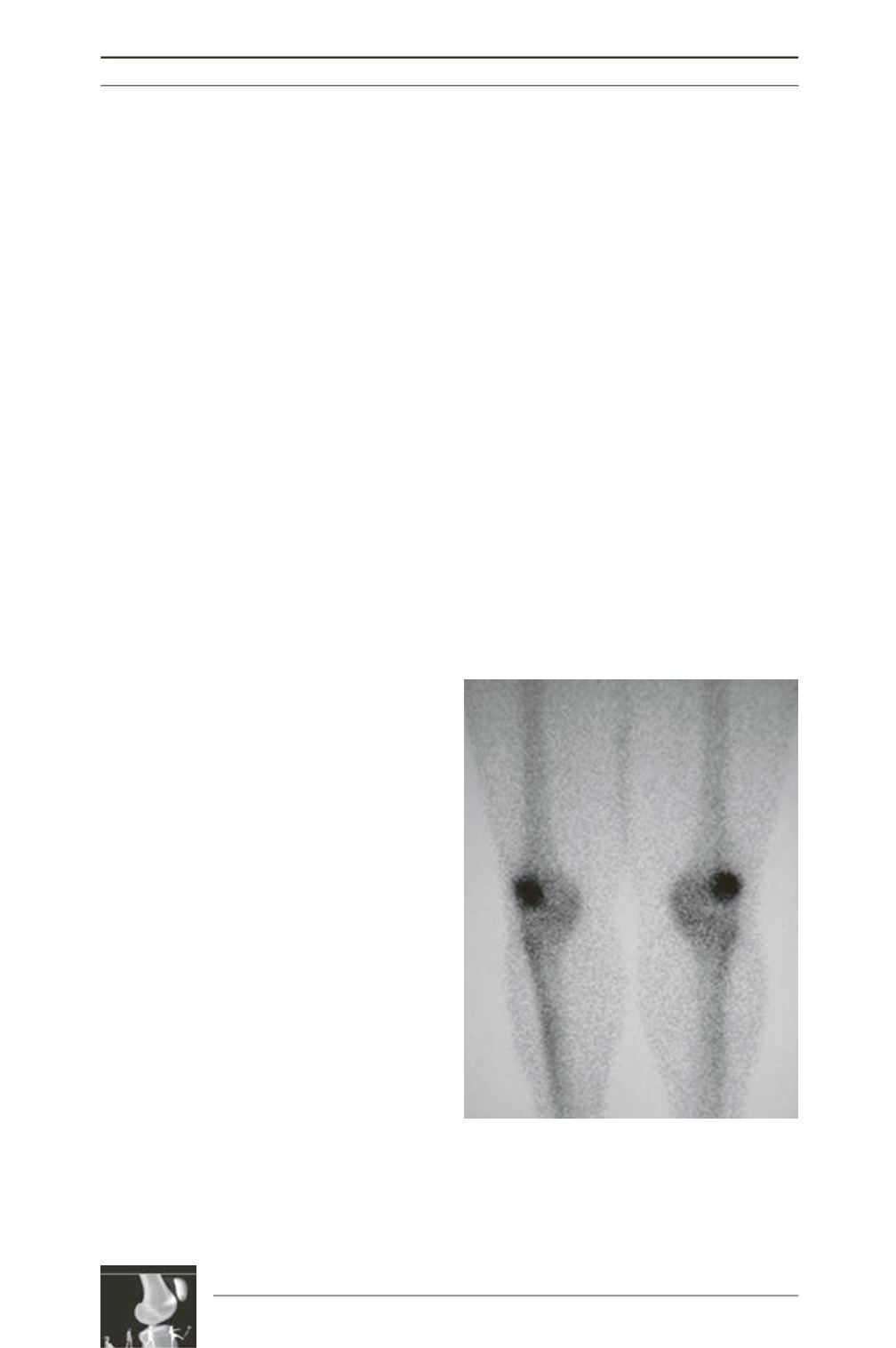
second development was Dye’s recognition
that radionuclear bone imaging could be a
useful tool in dynamically visualizing Wolf’s
Law. His concept of the comfortable knee and
patellofemoral joint functioning in a
homeostatic load/use envelope and the
association of patellofemoral pain with
supraphysiologic load in the absence of other
structural damage helped clarify an old dilemma
as to why isolated chondromalacia was not
always symptomatic [22] (fig. C). As a
corollary, while an inactive nuclear bone scan
can be seen in the painful degenerative
patellofemoral joint, an active nuclear bone
scan is not pathognomonic of a degenerative
diagnosis as some would claim.
Fig. C: Typical radionucleotide scan revealing loss
of bone homeostasis of the patellae. Plain
radiographs were normal; however, such patients
may or may not have patellofemoral degeneration.











