
Imaging in patellofemoral instability
29
3)
The patellofemoral index is the ratio (M/L)
between the thickness of the medial joint
space (M) and the lateral joint space (L),
measured on 20° axial views (Laurin). It
should measure 1.6 or less [22, 23].
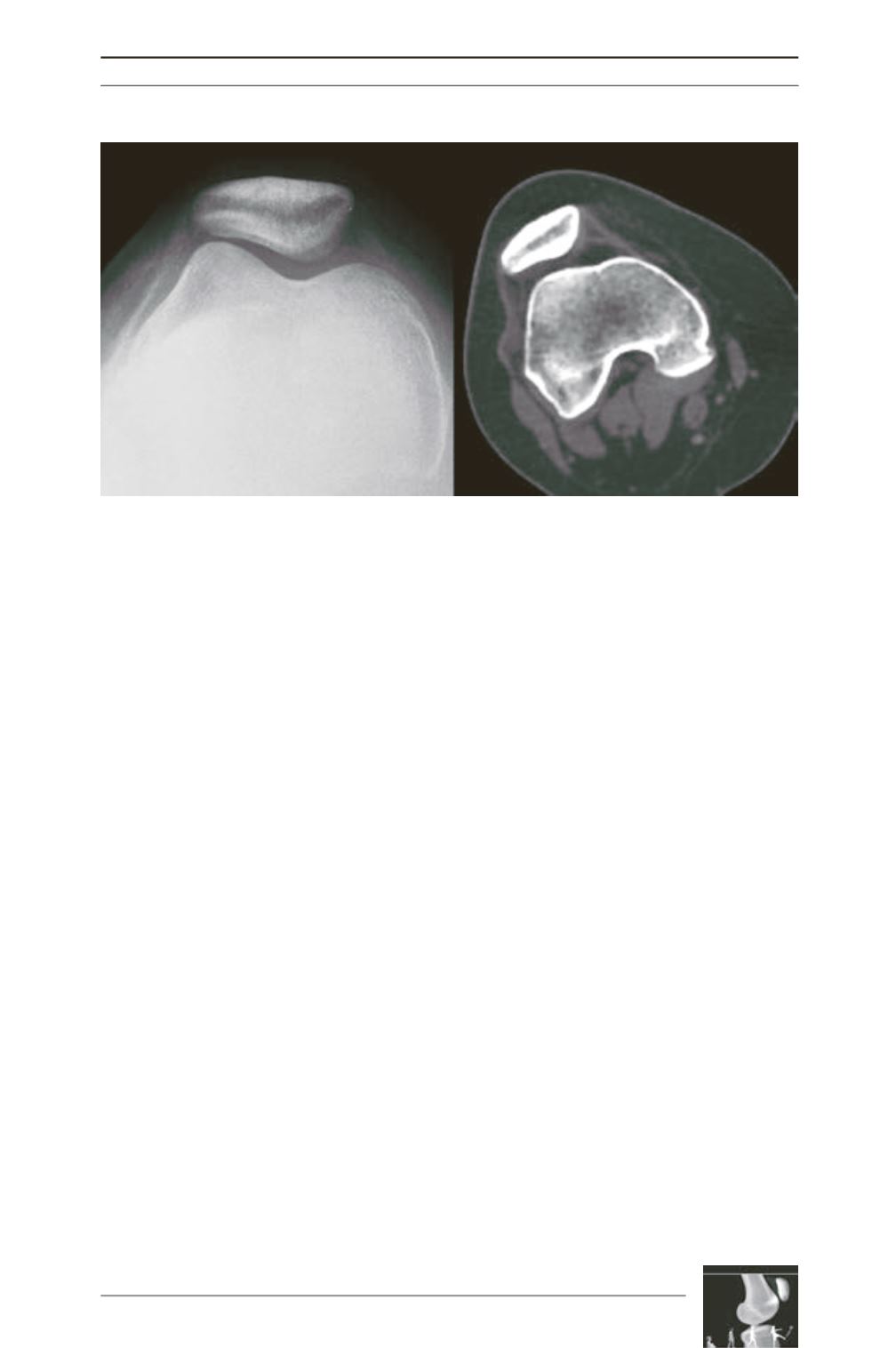
CT scans allow tilt measurements in complete
extension, which increases sensitivity because
as the knee flexes, trochlear engagement of the
patella reduces or corrects tilt and subluxation
(fig. 5). Another important contribution of CT
scans is that they allow tilt measurements to be
performed with a constant reference – the
posterior femoral condyles (versus the variable
trochlear shape in the instability population
observed in X-rays). According to Lyon’s
Protocol [1] patellar tilt is the angle formed by
the transverse axis of the patella and a tangent
to the posterior femoral condyles. It must be
measured with and without quadriceps
contraction, and this can be accomplished
either with two superimposed cuts or with a
single cut that images both references. Values
above 20° are considered abnormal.
In H. Dejour’s study, 83% of the objective
patellar dislocation group have patellar tilt
superior to 20° compared to 3% in the reference
normal group. If instead of using only the
relaxed quadricepsmeasure amean is calculated
between the measures performed relaxed and
in contraction, and the threshold value remain
the same, sensitivity and specificity are
improved. Ninety percent of the objective
patellar dislocation population have presented
values over this, while the same remains true
for only 3% of controls [1].
Acute dislocations
Imaging of acute dislocations is useful to
confirm the diagnosis and define treatment.
X-rays are useful to identify gross instability
and incongruence. Antero-posterior, lateral and
axial views are complementary and must be
performed. Fragments of the patella or the
lateral femoral condyle can be identified after
acute dislocations and may indicate surgical
treatment. CT findings in acute dislocations are
similar to the X-ray ones, but with increased
accuracy. Smaller osseous fragments can be
identified and better measured.
Patellar dislocation may not be suspected
before MRI examination in up to 50% of cases
[24]. MR imaging is particularly helpful in
Fig. 5: Patellar tilt and trochlear dysplasia were clearly depicted
on axial CT imaging (at full extension), but missed on the axial X-ray.











