
Imaging in patellofemoral instability
27
using the patellar tendon: patella ratio. On
sagittal MR imaging, patella alta is suggested
at values greater than 1.3. Neyret
et al.
[17]
measured with radiographies and MRI the
patellar tendon length in 42 knees with history
of patellar dislocation and 51 control knees.
They concluded that patella alta is caused by a
long patellar tendon rather than by its abnormal
insertion into the tibia. Additionally, they did
not found any significant difference between
X-ray and MRI tendon length measurements.
Other methods of measuring patellar height use
the trochlea as the reference. Bernageau [18]
described a method on lateral X-rays with the
knee in extension and the quadriceps contracted.
If the inferior edge of the articular surface of
the patella (R) is more than 6mm above the
superior limit of the trochlea (T) there is patella
alta, and if R is more than 6mm beneath T there
is patella baja. Biedert and Albrecht [19]
described the patellotrochlear index on sagittal
cuts of MRI, performed with the knees in
extension, the foot 15° externally rotated and
the quadriceps consciously relaxed. To calculate
the index, first we must measure the length of
the articular cartilage of the patella (baseline
patella: BLp). The second measure is the length
from the trochlear most superior aspect to the
most inferior part of the trochlea facing the
patellar articular cartilage (BLt). The ratio BLt/
BLp is calculated in percentages, and values
above 50% indicate patella baja while values
inferior to 12,5% indicate patella alta.
Tibial tubercle –
trochlear groove
distance (and torsional
measures)
TT-TG is a simple way to measure the valgus
(lateralizing) forces acting on the patella. This
distance is able to quantify the coronal
alignment of the extensor mechanism, or what
is called in clinical evaluation the “Q-angle”.
Originally, TT-TG has been described by
Goutallier and Bernageau [20] on X-ray axial
views, but it was popularized as the distance
from the bottom of the most proximal part of
the trochlear groove to proximal part of the
tibial tubercle, measured with two CT
superimposed cuts and expressed in millimeters
[1]. The first cut (reference cut) is through the
proximal trochlea, identified by a slight
condensation of the lateral facet and by the
shape of the notch (rounded, looks like a roman
arch). The second cut goes through the proximal
part of the tibial tubercle. The deepest point of
the trochlear groove and the central point of the
tibial tubercle are projected on a line tangential
to the posterior femoral condyles and the
distance from each other is measured. The
normal mean value in a control population is
12mm; in the population with objective patellar
dislocation the value is superior to 20mm in
56% of the cases [1]. Values above 20mm are
considered abnormal.
Another important contribution of CT produced
by the superimposition of images is the
assessment of torsional deformities, such as
femoral anteversion and external tibial torsion.
Femoral anteversion is increased in patients
with instability (15,6±9 vs. 10,8±8,7 in normal
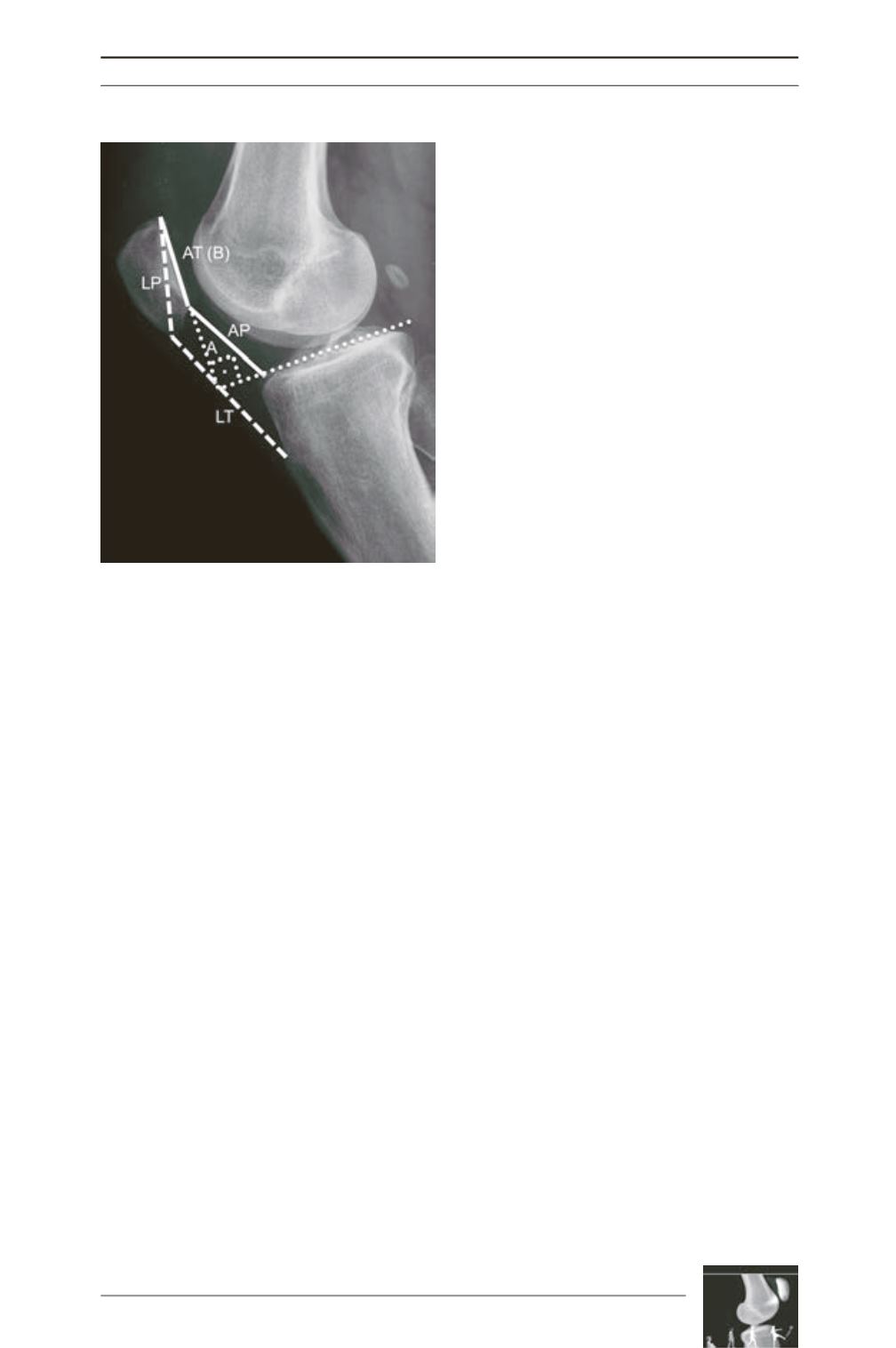
Fig. 2: Patellar height measurement methods
(using the tibia as reference) on the lateral view.
Caton and Deschamps (AT/AP), Insall and Salvatti
(LT/LP) and Blackburne-Peel (A/B).











