
Whether to resurface the patella in total knee arthroplasty
341
Discussion
Despite numerous publications, still today,
opinions differ concerning patellar resurfacing.
Even if several prospective randomised studies
were able to identify a lack of significant
difference [1, 3, 4, 6], numerous other series
and authors put forward the contrary opinion
[9, 10, 12, 14, 15], each of the techniques being
subject to its own risks [5, 7, 8, 11]. Some of
these divergences come from the same
evaluation of patients in each series [2]. Bonin
et al.
moreover advise using subjective scores
rather than the IKS to better pinpoint the
patellofemoral origin of the pain.
Few studies have been concerned with the
consequences of choice of implant; Waters
et
al.
[13] attempted to bring to light a change in
the post-operative results dependent on the
shape of the trochlea inserted. If this shows that
anterior pain appears more relevant in the case
of non-resurfacing, it also underlines the fact
that this pain would seem more relevant in the
case of “inhospitable” trochlear shape,
particularly in the case of trochlear crossover
and asymmetry.
In our case study, the prosthesis utilised is a
prosthesis initially designed to harbour a dome-
shaped polyethylene patellar component, with
a constant radius of curvature of the femoral
plate over the entire contour, allowing us to be
assured that the purely
static conditions of con
gruency, for an identical
patellar cross-section, re
main unchanged at an
angle of flexion other than
the chosen 45°.
Despite the significant
depth of the femoral plate
selected,
contrary
to
Waters, there is no evi
dence for much patello
femoral pain. We appear to
encounter this pain prima
rily in cases of Wiberg
3 patellae.
Patellae with shapes classed as Wiberg 1 and 2
appear to benefit from flexibility of adaptation
to the trochlea both arthroscopically and
radiographically as well as clinically. They
indeed possess a certain degree of rotational
and translational freedom on the axial plane,
sufficient, taking into account their shape, to
obtain a stable patellofemoral pair. Will this
“constrained” adaptation be confirmed over the
long term?
Our study has already revealed the clinical
outcome at one year of these constraints in the
case of initial “major incongruency”. Thus pre-
operative detection of these future “major
incongruencies” would be of interest, in order
not to promote the occurrence of premature
pain.
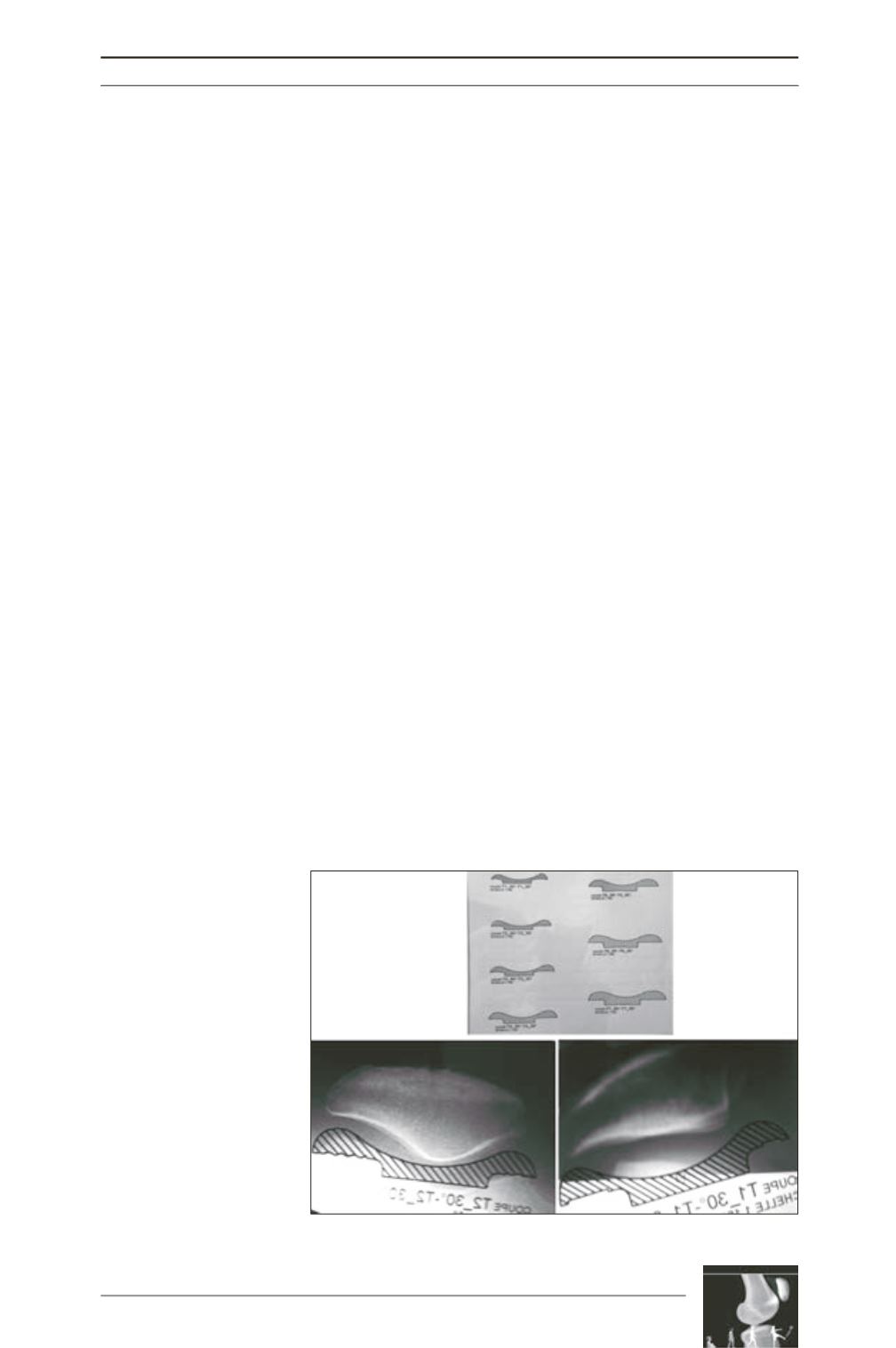
We suggest pre-operative planning, using
drawings of transverse sections of the prosthetic
femoral plate. These drawings, applied to a
systematic patellofemoral contour, would allow
verification of the absence of major
incongruency with the native patella, and thus
the need to review the decision for resurfacing
or patelloplasty (fig. 5).
Good congruency in this case during planning,
non-resurfacing method can be suggested. By
contrast, in the caseof predictable incongruency,
it will doubtlessly be wiser to perform
resurfacing of the patella or patelloplasty.
Fig. 5











