
D.C. Fithian
94
As the clinician develops an understanding of
the symptoms and complaints, he or she can
begin to develop one or more hypotheses,
which can be tested in the physical examination
and with subsequent imaging studies. The
isolated complaint of pain, with no objective
findings to suggest a specific source (pathology)
representing an indication for surgery, should
be treated nonoperatively.
Physical examination
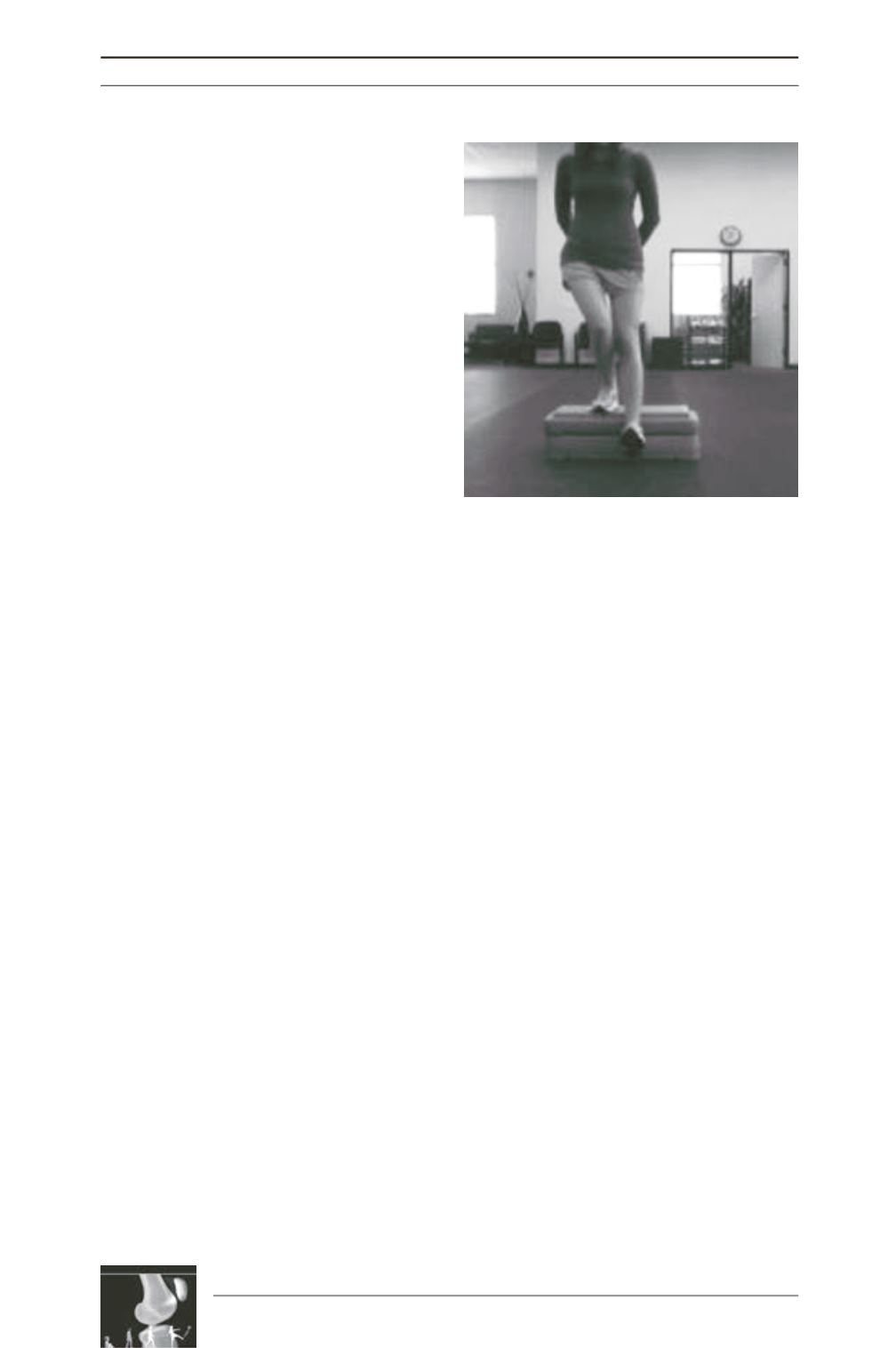
Due to the complex and delicate interactions
between the knee extensor system and lower
limb function, clinical evaluation of patello
femoral complaints can be challenging. After
other disorders have been ruled out, specific
testing for disorders of the patellofemoral joint
can be performed. The patient should be
evaluated standing, walking, and stepping up
and down from a small step, squatting, sitting,
supine, running, and jumping. Observation of
the patient during a few functional activities
yields a great deal of information about patello
femoral loading and neuromuscular condi
tioning (fig. 1). Any hindfoot valgus, forefoot
pronation, and/or heel cord tightness should be
noted as they can affect tibial rotation and
patellofemoral alignment [1].
The prone position allows estimation of several
important variables, including quadriceps
tightness (important if correction of patella alta
is being considered), femoral internal and
external rotation limits, and foot-thigh angle
(FTA) and/or trans-maleolar axis (TMA)
(fig. 2). Femoral and tibial rotation can be
estimated by examining the patient prone with
the hips extended, the knees flexed 90°, and the
feet and ankles in a neutral, comfortable
position with the soles of the feet parallel to the
floor after the method of Staheli
et al.
[2]. Kozic
et [3] showed that on physical examination,
femoral anteversion should be suspected if
prone hip internal rotation exceeds external
rotation by at least 45 degrees. With respect to
estimating FTA and TMA, Staheli reported a
wide range of normal values, with mean values
of 10° for FTA and 20° for TMA [2]. Souza and
Powers also confirmed the reliability of the
Staheli method for estimating femoral
anteversion, though axial imaging was more
precise [4]. Our preferred approach is to use the
prone physical examination to screen for torsion
of the tibia and femur, and to obtain CT scan to
assess rotational alignment if hip IR exceeds
ER by at least 20 degrees or if the prone foot-
thigh axis or TMA is greater than 20 degrees.
The lines of action of the quadriceps and the
patellar tendon are not collinear. The angular
difference between the two is the quadriceps
angle, or “Q-angle”. Because of this angle, the
force generated by the quadriceps serves to
both extend the knee and to drive the patella
laterally, compressing the femoral trochlea in
order to convert tension in the quadriceps into
extension torque at the knee. The relative
magnitude of the laterally directed force is
related to the Q-angle. External rotation of the
tibia, internal rotation of the femur, and
increasing knee valgus all cause an increase in
the Q-angle and thus an increase in the laterally
directed force within the PFJ (fig. 3) [1].
Fig. 1: The step-down test is a simple test that can be
done in the clinic to evaluate core and hip control.
This patient demonstrates pelvic weakness with hip
adduction and medial collapse of the knee. It is
apparent that her weakness results in a variety of
functional alignment abnormalities, including: (1)
contralateral pelvic drop, (2) right femoral internal
rotation, (3) right knee valgus, (4) right tibia internal
rotation, and (5) right foot pronation.











