
The Clinical Examination in Patellar Instability
97
be symmetric in each direction and not exceed
7-10mmwith a 5-lb load [11, 13]. Alternatively,
the patella can be divided into 4 quadrants and
the displacement can be recorded in quadrants.
Particularly in heavy patients, stress xrays may
be more useful for assessing patellar mobility
[14]. If patients are apprehensive as the patella
is moved, an exam or stress X-rays under
anesthesia can be very helpful to confirm
pathological laxity prior to proceeding with
surgical stabilization. Stabilization is never
indicated unless excess laxity has been
documented either in the clinic or under
anesthesia.
Summaryand
Conclusion
The history and physical examination are key
to understanding a patient’s presenting
complaint, and for determining further workup
and treatment. This chapter focused on the
physical features of patients presenting with
complaints of knee pain and instability. It is
important to realize that meniscus tears,
cartilage flap tears and ligament insufficiencies
other than MPFL laxity sometimes result in a
patient being referred for treatment of patellar
instability. It is the responsibility of the
consultant to identify MPFL laxity prior to
embarking on any surgical treatment for
supposed patellar instability. At this time,
patellar instability can be documented only by
clinical examination or by stress radiography.
While several ancillary points of physical
examination are raised in this chapter, these
should not distract our focus from the primary
point of the chapter. Excessive laxity of patellar
constraints, principally of the MPFL, is the sine
qua non of patellar instability. No patient
should undergo patellar stabilization unless the
clinical workup has demonstrated deficient
constraint of medial or lateral patellar motion
with respect to the trochlear groove.
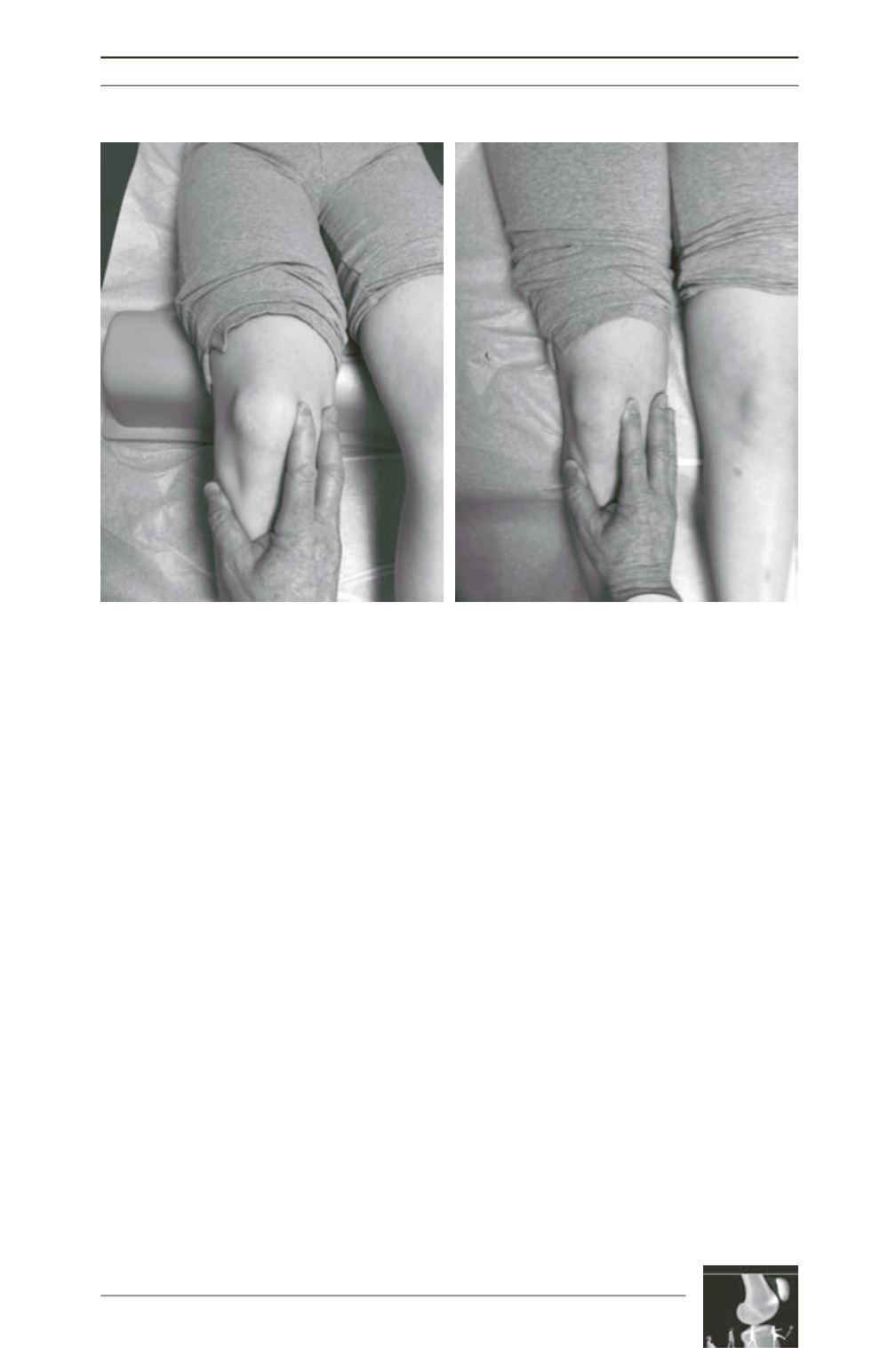
Fig. 4: (A) At 30º of flexion the patella is seated in the trochlear groove and it is easier to quantify the
amount of mobility in each direction (medially and laterally) [11]. Normal translation should be symmetric
in each direction and not exceed 7-10mm with a 5-lb load [11, 13]. (B) The checkrein, or endpoint of MPFL
laxity usually is easier to recognize at 0º because in this position the trochlea does not constrain the
patella, so it is easier to feel an “endpoint” as you displace the patella laterally [12]
A
B











