
Revisions of UKA with TKA; Medial versus Lateral UKA
211
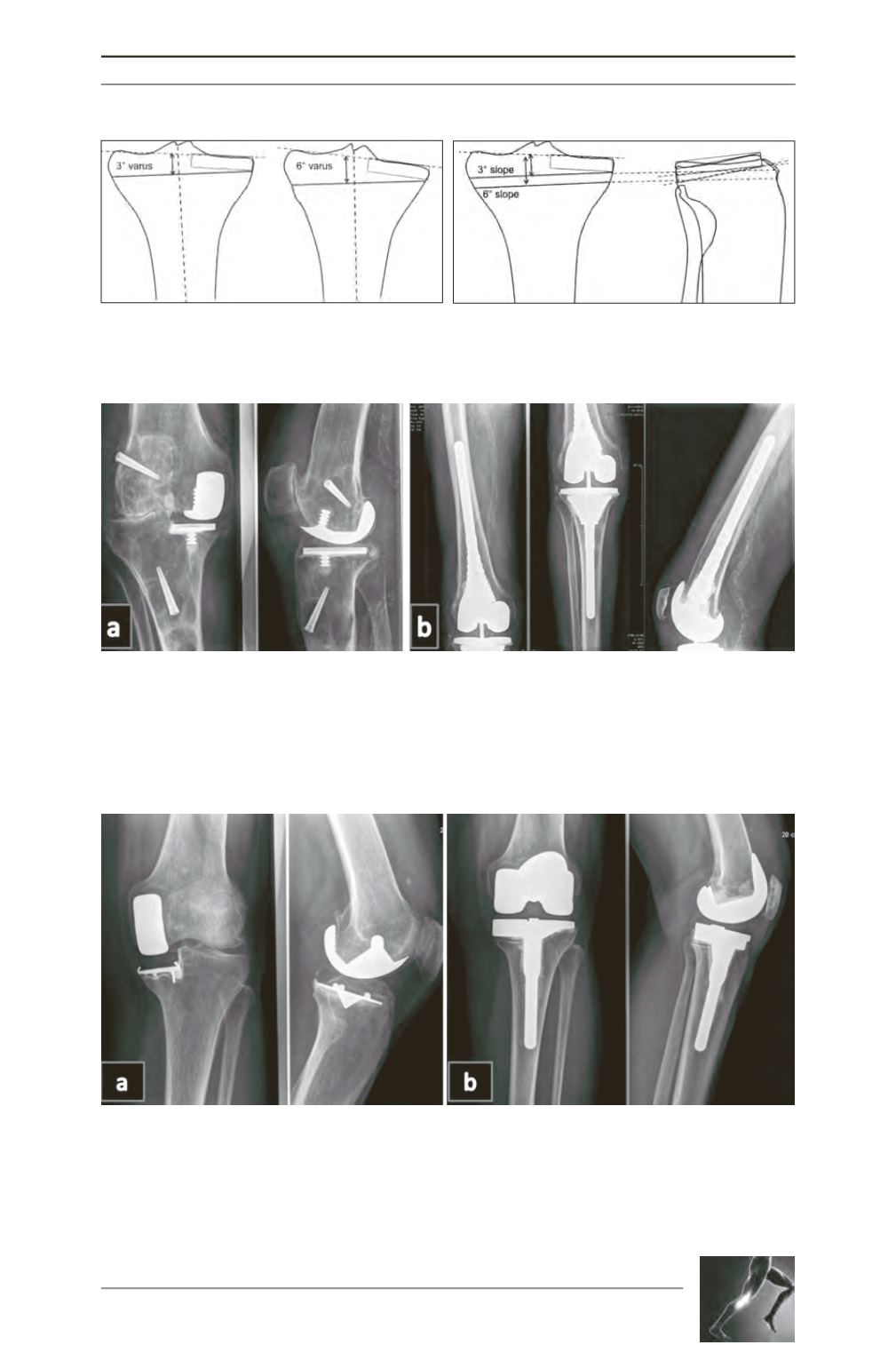
Fig. 1: Effect of varus cut on resection level.
Fig. 2: Effect of angle of resection
on potential bone cuts.
Fig. 3: Demonstrates a case of an 84yo man, presenting with severe knee pain 20 years after a medial UKA.
Of note he had an ACL reconstruction using a synthetic graft 10 years prior to that intervention. Imaging
showed a massive area of lysis (fig. 3a), and once an infective cause was outruled, a revision of UKA to TKR
was undertaken encompassing curettage of the granuloma and insertion of a constrained long stemmed
revision prosthesis (fig. 3b). Although an indirect – an unusual – cause of failure for a UKA, this case
highlights the difficulty of balancing resection minimization with obtaining stable fixation.
Fig. 4: Shows a clinical case of a 57 year old lady, who presented to our service two years with ongoing
medial knee pain following a UKA to UKA procedure, which had been performed for persistent pain which
corresponded to a site of lysis and bony sclerosis under the medial tibial plateau. Both the pain and the
radiographic lysis persisted after her UKA to UKA procedure (fig. 4a), and for which she had a UKA to TKA.
Although resection was as conservative as possible through the sclerotic medial tibial bone, and medial
augments used with a stemmed prosthesis, and clinical symptoms have improved, the area of lysis persists
at one year following her revision to TKR (fig. 4b).









