
W. Fitz
92
New surgical techniques try to approximate the
restoration of the femoral and tibial anatomy
called “shapematching” [6, 7] which challenges
principals of TKR such as tibial components is
in too much varus. “Shape matching” does not
improve knee kinematics [8].
Current surgical techniques do not restore the
posterior medial condyle. With more femoral
external rotation the amount of resected posterior
medial condyle exceeds implant thickness
(fig. 3). Moving the pivot point to the surface of
the posterior medial condyle and resecting the
implant thickness off the posterior medial
condyle would restore the medial condyle and
decrease the looser lateral flexion gap (fig. 3).
Matching the proximal tibial varus and valgus
angle using a symmetric tibial implant results
in substantial numbers of tibial components
placed in more than 3 degrees of varus [7].
Custom TKAaddress
shortcomings of
off-the-shelf implants
Custom implants address high variability and
range of different AP and ML dimensions.
Asymmetric anatomic condylar geometries
restore the distal femoral condylar anatomy.
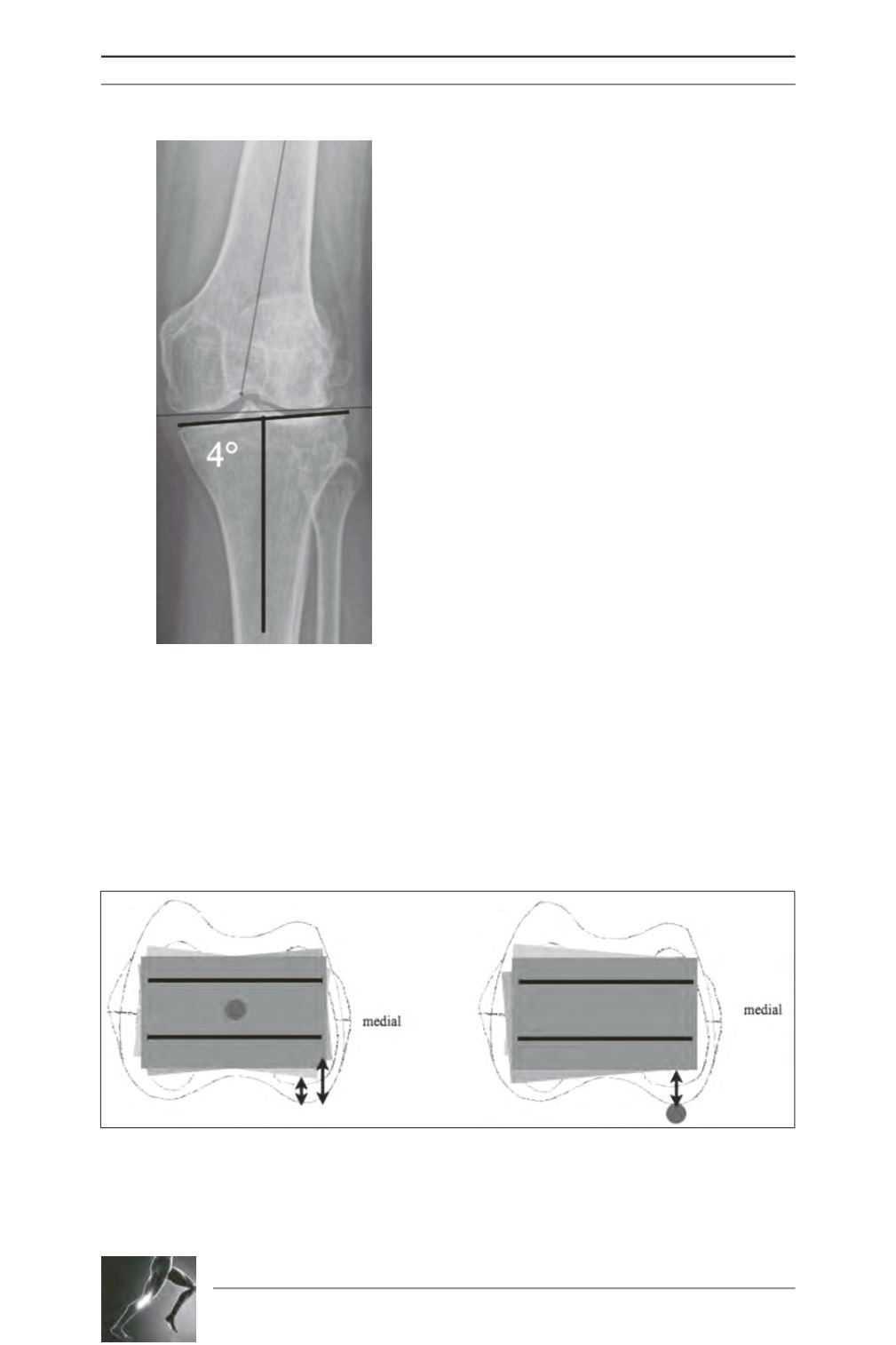
Fig. 2: The proximal tibial condyle
has a large range of varus or
valgus. Comparing osteoarthritic
(n=80) with non-osteoarthritic
patients (n=356) the mean was
1.1° varus ± 1.2° (6° varus to 3°
valgus) in the osteoarthritic group
and 0.8° varus ± 1° (4° varus to 4°
valgus) in the control group 14.
Fig. 3: The pivot point for femoral rotation is in the center of the distal femur and external rotation of the
femoral component results in increased bone resection of the medial condyle and less of the lateral
posterior condyle not matching the implant thickness. Moving the pivot point to the posterior surface and
resecting the implant thickness off the posterior medial condyle would restore the medial condyle and
decrease the looser lateral flexion gap.









