Prosthetic tibial stems were required for both
the study and control groups. A longer tibial
stem was used in 10 cases of the study group
and in 5 cases of the control group (p=0.2). The
tibial cut thickness was over 9 mm in 8 cases of
the study group and 7 cases of the control group
(p=0.8). An augmentation of the polyethylene
insert thickness was necessary in 10 cases of the
study group and 5 cases of the control group to
obtain appropriate laxity (p=0.2).
There were references in the TKA operative
notes which described increased technical dif-
ficulty secondary to the previous ligament
injury. We observed two intra-operative com-
plications in the study group corresponding to
the exposure: one patellar tendon partial avul-
sion and one femoral fracture (condylar fractu-
re). No intra-operative complications were
observed in the control group.
In the early postoperative period, one mobili-
zation under anesthesia was required in the
study group for a lack of flexion and none in
the control group.
The mean follow-up after TKA in the study
group was 37 months (20-153 months), and
the control group was 40 months (19-103
months) (p=0.4).
Preoperatively, the mean loss of extension
was 3.5° ± 4 (0-15) and 5° ± (0-30) in the
study group and the control group, respective-
ly (p=0.4). The mean flexion was 119° ± 17
(50-150) and 118.5° ± (30-160) (p=0.9). The
mean IKS knee score was 43 ± 20 (0-89) and
43 ± 17 (2-74) (p=0.9). The mean IKS func-
tion score was 63 ± 17 (15-100) and 61.5 ± 18
(15-100) (p=0.5).
TOTAL KNEE ARTHROPLASTY: A SAFE AND EFFECTIVE PROCEDURE FOR ADVANCED OSTEOARTHRITIS…
309
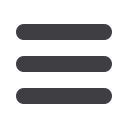
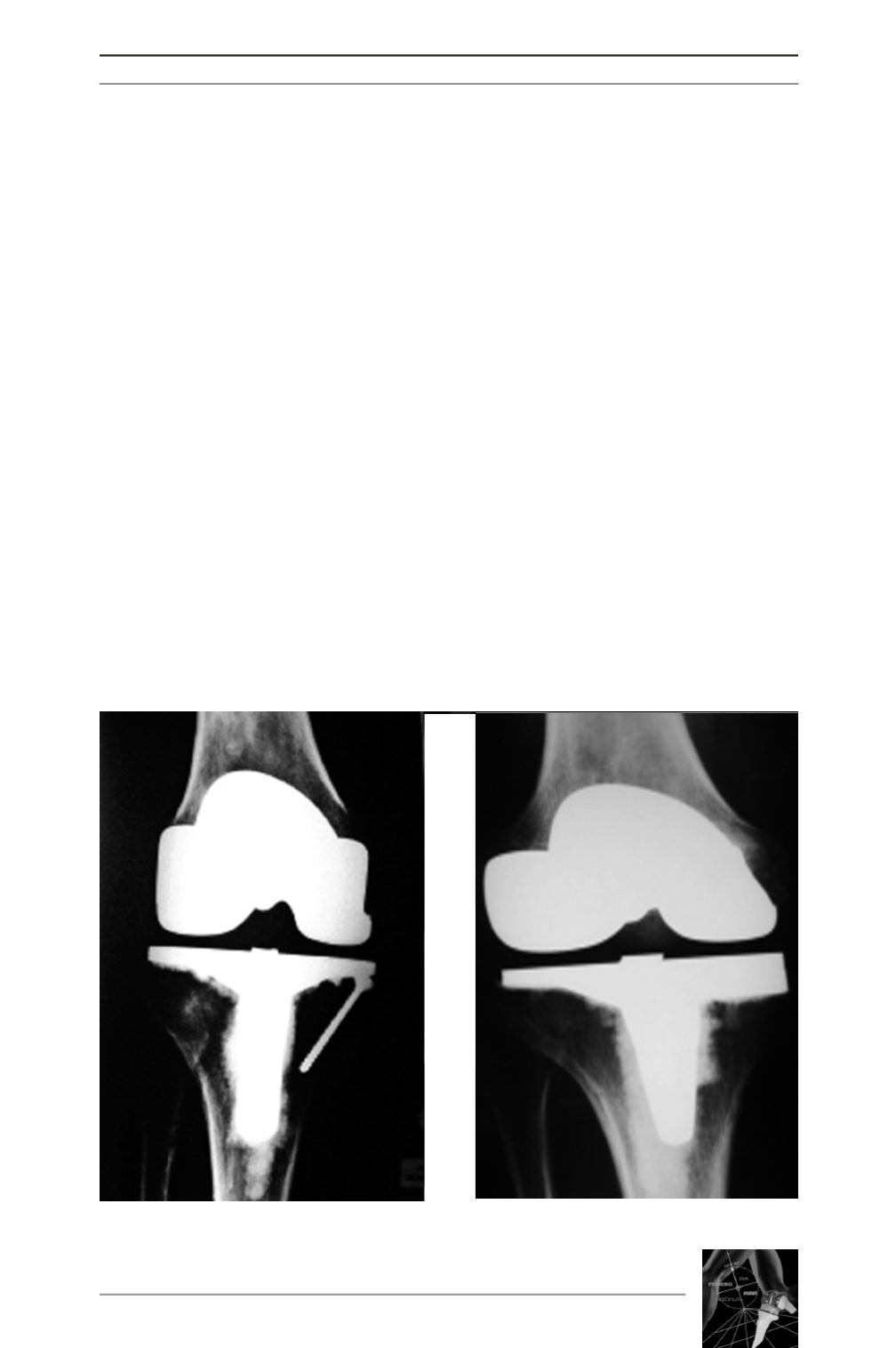
Fig. 1 : Bony defect management using screw or medial tibial wedge











