
M. Thaunat, C. Bessiere, N. Pujol, P. Boisrenoult, P Beaufils
200
recession wedge trochleoplasty is a safe
procedure for patellar instability with major
dysplastic trochlea, and effective in preventing
future patellar dislocation and in reducing
anterior knee pain. Since this procedure may
reduce patellofemoral joint reaction force
without modifying patellofemoral congruence,
it should also prevent late patellofemoral
degeneration.
Methods
Patients
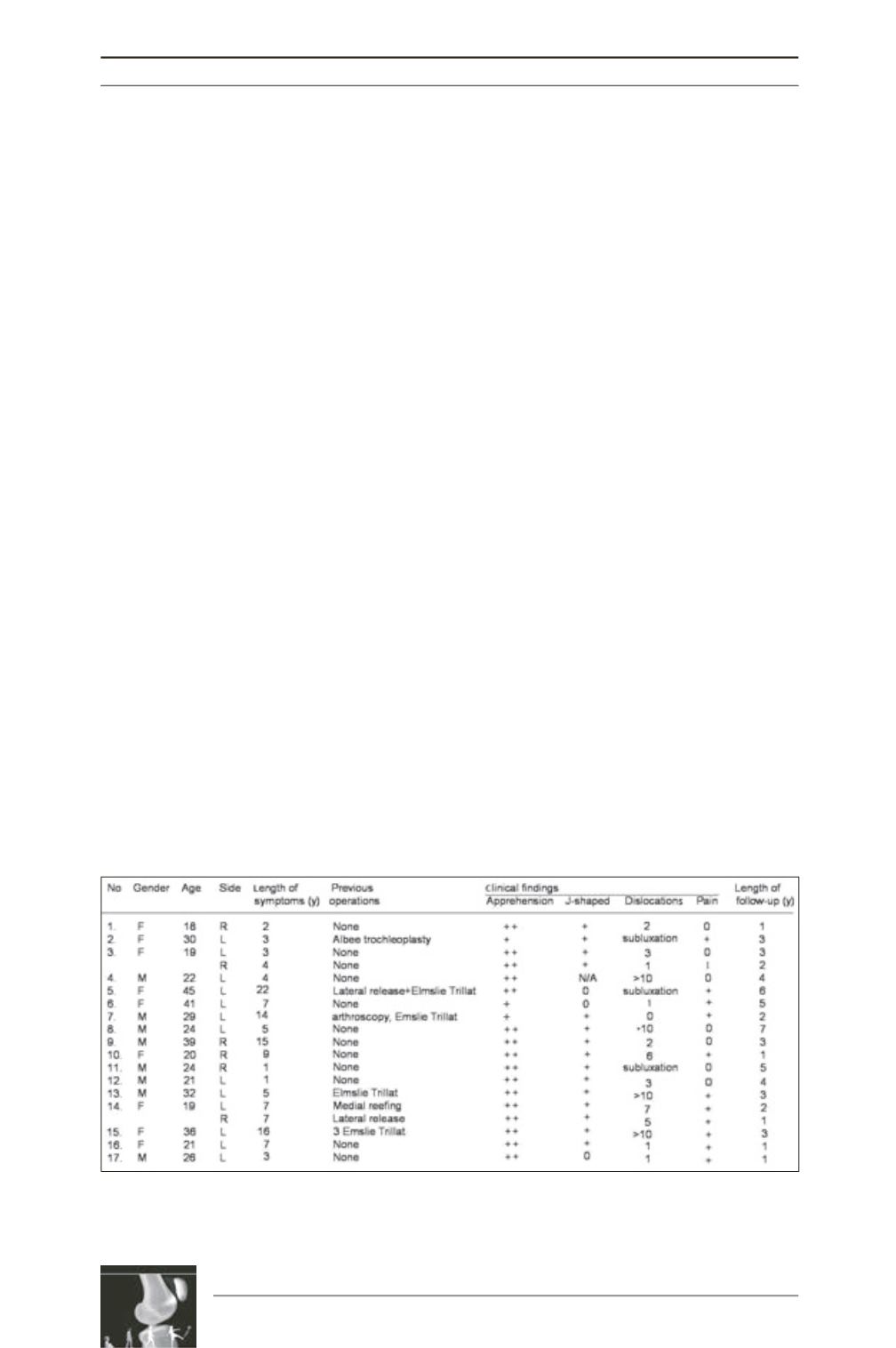
Between April 2004 and March 2009, 20
depression trochleoplasties were performed by
three different surgeons in our department on
18 patients (10 female, 8 male; 13 left knees,
7 right knees). One patient could not be
contacted for reassessment and was considered
lost to follow-up; 17 patients (19 knees) were
assessed at last follow-up. Mean age at
operation was 23 years (range, 18 to 45 yrs).
Mean symptom duration before trochleoplasty
was 7 years (range, 1 to 19 yrs); 7 knees had a
total of 15 previous operations (Table 1).
Indications for surgery were either
patellofemoral instability (n=14) or pain (n=5).
Patellofemoral instability was defined as
recurrent subluxation (n=3) or recurrent
dislocation (n=11) associated with dysplasia of
the femoral trochlea. Dysplasia was defined by
positive crossing sign and a trochlear bump,
according to theDejour andWalch classification
(fig. 2) [7]. Persistent retropatellar pain and
crepitus due to trochlear dysplasia was the
indication in the remaining patients, who
experienced either only 1 dislocation (n=4) or
apprehension without dislocation (n=1). All
patients had failed to respond to conservative
treatment. Trochleoplasty was never isolated
but associated to either realignment of the
extensor apparatus or MPFL reconstruction,
according to the “à la carte” surgery concept.
Surgical treatment addressed each of 4 principal
factors whenever present: trochlear dysplasia,
tibial tubercle-trochlear groove offset (TT-TG),
patella alta, and/or patella tilt. All patients were
assessed clinically and had plain radiographs
and CT scans. Plain radiographs in this study
included weight-bearing AP view, non-weight-
bearing lateral view and Merchant view. As
long leg standing X-ray was not included in the
preoperative planning, the mechanical axis of
the leg could not be determined. Lateral views
were used to measure patellar height, according
to the Caton-Deschamps method [8] (normal
range, 0.6 to 1.2), and trochlear dysplasia.
Merchant views were used to measure patellar
tilt angle (PTA), the angle subtended by a line
between the edges of the patella and the
horizontal; a line along the subchondral bone
of the anterior patella can be substituted for the
edge-to-edge line [9]. CT was used to measure
Table 1: Patient demographics. Patellar apprehension was graded from 0 to ++: 0, no apprehension; +,
discomfort on extreme lateral translation of the patellar in extension, or true apprehension with voluntary
quadriceps contraction on lateral translation in extension; and ++, when the patient stops the clinician
touching the patella.











