
Recession wedge trochleoplasty for major trochlear dysplasia
205
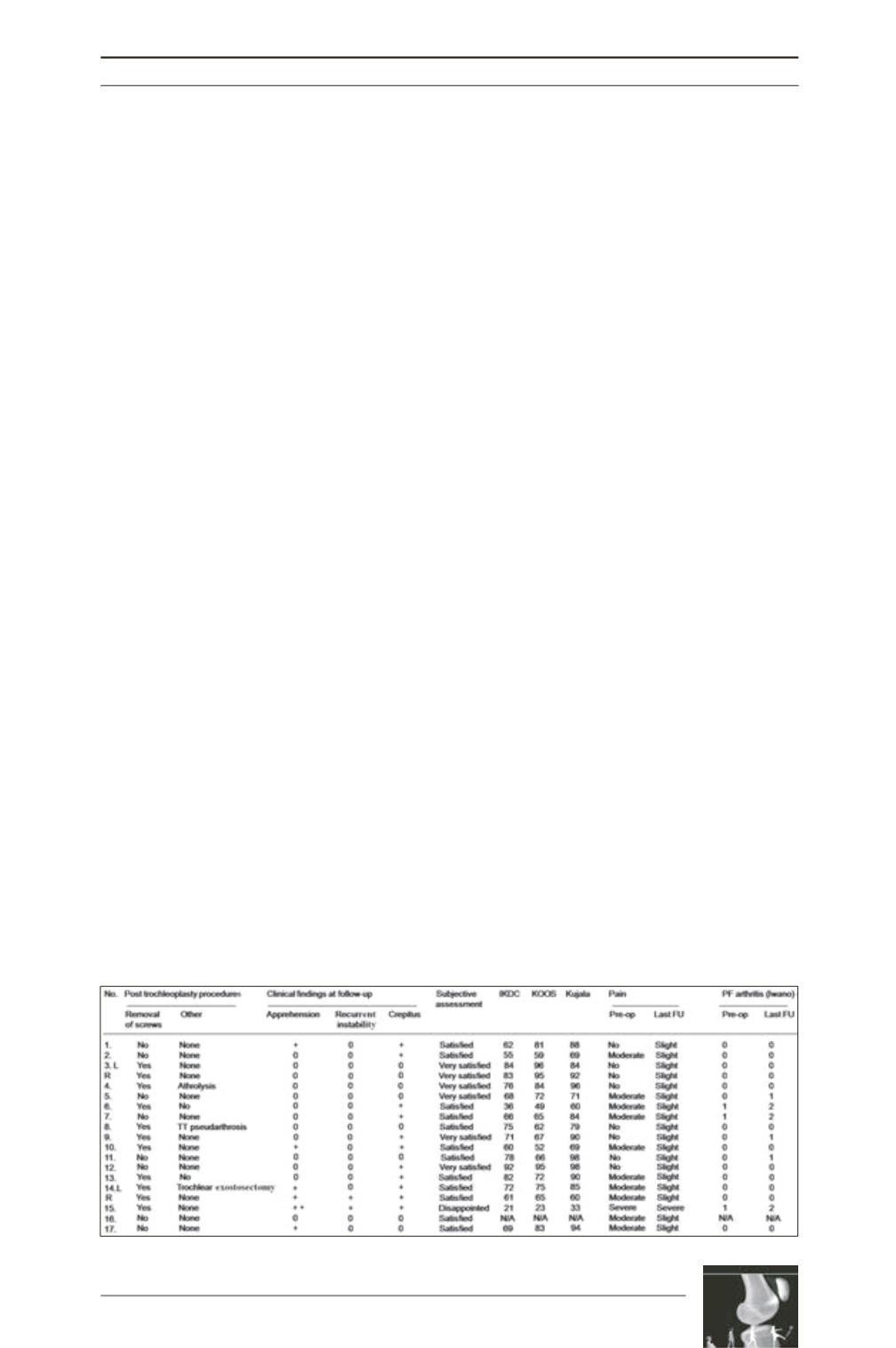
All patients operated on for painfree instability
(n=7) had slight pain at last follow-up. The
pain was generally localized around the tibial
tubercle screw sites. All patients, except 1 who
complained of pre-operative pain, (n=11)
reported significant pain improvement at last
follow-up (Table 3).
The operation failed to stabilize the
patellofemoral joint in 2 cases. One had a fall,
sustaining dislocation of the patella, managed
conservatively without further episodes of
instability. One patient had recurrent patello
femoral instability; she had had 3 tibial tubercle
transpositions before the operation but was still
in pain and unstable, and remained unchanged
after the index operation; she was the only
patient who declared she was disappointed by
the operation.
Radiological outcome
Mean trochlear groove height (BC) changed
from 4.8mm (range, 0 to 8mm) pre-operatively
to -0.8mm (range, -8 to 6mm) post-operatively,
and mean trochlear ridge height (AC) from
9.1mm (range, 5 to 13mm) to 3.4 mm (-4 to
11mm). Mean PTA on Merchant view changed
from 14° (range, 6° to 26°) to 6° (range, -1° to
24°). There was no significant difference in
PTA correction according to associated
MPFL reconstruction. Six patients showed
radiological signs of patellofemoral osteo
arthritis at last follow-up. Radiological changes
appeared in 3 patients and the 3 cases of pre-
operative Iwano grade 1 [16] scored as grade 2
at last follow-up.
Discussion
The most important finding of the present study
was that recession wedge trochleoplasty is
feasible as an additional procedure for patellar
instability with major trochlear dysplasia. The
ideal indication for recession wedge
trochleoplasty is painful patellofemoral
instability with major trochlear dysplasia
(grade B, C or D on Dejour’s classification,
with trochlear prominence >5mm), or when
other procedures have failed to provide
patellofemoral stability. Depression trochleo
plasty seems to prevent future patellar
dislocation and is effective in reducing anterior
knee pain in these difficult primary cases or in
revision when other realignment procedures
have failed. It also provides improvement in
radiographic measurements, including a
decrease in trochlear prominence and patellar
tilt angle. The present results are similar to
those of several investigators in terms of
improved subjective short-term outcome scores
[2, 6, 17-21] (Table 4). However, comparison
with other series is difficult since surgical
procedures and follow-up varied, numbers
were often small and patients were sometimes
treated for pain rather than instability [6, 21]. It
is not possible to assess the role of trochleoplasty
in patellofemoral stability, as it was never
Table 3: Further postoperative procedures, clinical findings at follow-up, and satisfaction scores.











