
M. Thaunat, C. Bessiere, N. Pujol, P. Boisrenoult, P Beaufils
206
isolated and associated abnormalities were
always corrected in the same surgical step. We
think, however, that correcting trochlear depth
abnormality plays a major role in stabilizing
the patella by facilitating proper entrance of the
patella into the trochlea. Depression
trochleoplasty was found to enable PTA
correction even when the MPFL was not
reconstructed, and is effective in revision when
other procedures had failed, as reported by
Goutallier
et al.
[6]. Thus, MPFL reconstruction
should not be necessary when recession wedge
trochleoplasty has been performed, as the
reduction in trochlear prominence prevents
lateral misdirection and facilitates patellar
sliding into the trochlear recess. The instability
recurrence rate of around 10% (n=2) in the
present series was acceptable, given that in 1 of
the cases trauma was implicated in the recurrent
patellar dislocation, and the other was a difficult
multi-operated knee in which three previous
stabilization procedures had already failed.
Deepening trochleoplasty is often not attempted
because of surgeons' limited familiarity with
this demanding surgical technique. There is,
moreover, no reliable landmark to determine
where to locate the new trochlear groove. In
comparison, recession wedge trochleoplasty
requires assessment of the abnormal geometry,
but is not difficult to master. Wedge recession
is identical in principle to deepening
trochleoplasty, except that a wedge rather than
a trench of bone is removed so as to create a
new sulcus. It was first described by Goutallier
and early results were encouraging [6]. The
aim is to lower the subchondral bone of the
trochlear groove at the anterior cortex of the
femoral shaft without modifying its shape.
A study performed on fetuses by Glard
et al.
suggested that the anatomic characteristics of
the patellar groove were integrated into the
genome during the course of evolution [22].
This would be in favor of a genetic origin for
patellar groove dysplasia. Postnatally, the
position of the patella in relation to the trochlea
plays a major role in the final shape of the
patella and trochlea, which develop congruent
articulating surfaces [23, 24]. Moreover, there
is a difference between the bony and cartilage
morphology of the patellofemoral joint [25,
26], so that congruent cartilaginous articulation
maycoexistwithunderlyingbonyincongruence.
From this point of view, lowering without
deepening the groove facilitates the entry of the
patella into its groove with respect to
patellofemoral congruence. The aim of the
procedure is to diminish the central bump
responsible for patellar misdirection and lateral
subluxation and to guarantee adequate trochlear
depth, and maximal hyaline cartilage
conservation without affecting patellofemoral
cartilage congruence.
The risks associated with deepening trochleo
plasty include breaking the osteochondral flap,
distal detachment, and excessive thinning of
the flap, decreasing blood supply. There are
also concerns about articular cartilage viability
following trochleoplasty. Recession wedge
trochleoplasty should decrease the risk of
chondral damage and necrosis. Since the
dysplastic segment of the trochlea is lifted as a
single osteochondral block and there is no need
to fashion a new groove by cutting the
osteochondral flap, it is possible to conserve
more subchondral bone, thus decreasing the
risk of possible severe irreversible articular and
subchondral injury, especially in older patients
where cartilage is less flexible. Moreover, the
wedge and trochlear recess are flat and
complementary, whereas in deepening trochleo
plasty, the osteochondral flap might not tally
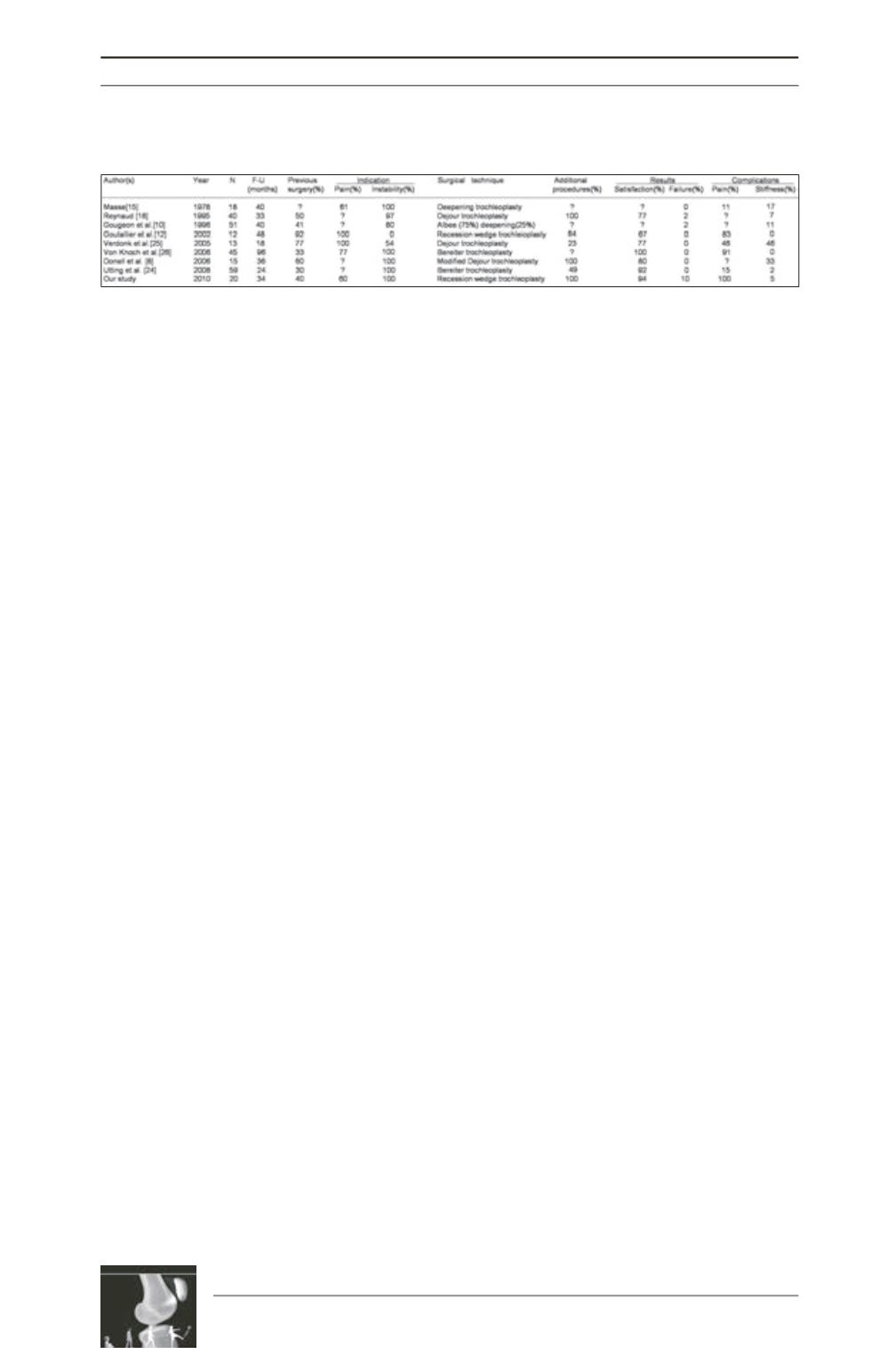
Table 4: Literature review: trochleoplasty for major dysplastic trochlea.











