
M. Thaunat, C. Bessiere, N. Pujol, P. Boisrenoult, P Beaufils
204
hardware removal; the patient maintained full
range of motion, and was satisfied at last
follow-up. One patient required arthroscopic
supratrochlear exostosectomy for a persistent
ridge causing pain without symptoms of
patellar instability; he too was satisfied, and
had no complaint at last follow-up. A further 8
operations were needed to remove anterior
tibial tubercle screws, due to pain over the
screw site; screws were also systematically
removed from the trochlea during the same
revision operation, although well tolerated.
One patient required 2 revisions for tibial
tubercle non-union, which healed with a
satisfactory result.
Clinical outcome
All patients except 1 were satisfied or very
satisfied by the operation. Functional outcome
on the various scores is summarized in Table 3.
Mean objective knee score at last follow-up
was 80 (±17) for the Kujala score, 70 (±18) for
the KOOS and 67 (±17) for the IKDC. Patients
with history of surgery, patellofemoral
chondropathy discovered during surgery (ICRS
grade ≥2) or degenerative change on pre-
operative radiographs tended to show lower
Kujala scores at last follow-up, but the
difference was not significant (fig. 4).
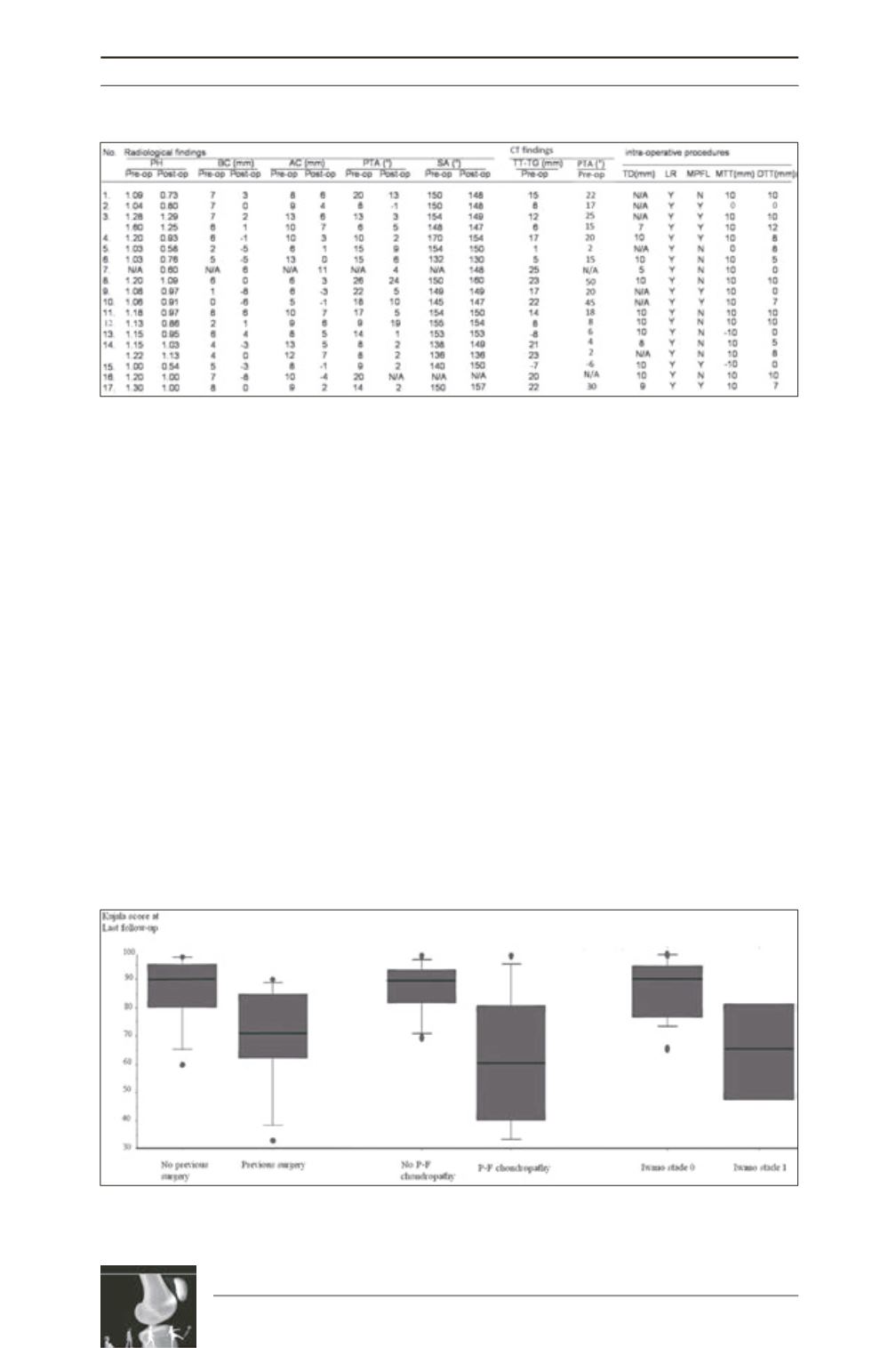
Table 2: Pre- and post-operative radiological results and operative details. PH=patellar height, BC=Boss
height, AC=Ridge height, TTTG=tibial tubercle–trochlear groove distance, PTA=patellar tilt angle,
SA=sulcus angle, TD=trochlear depression, LR=lateral release, MPFL=medial patellofemoral ligament,
MTT=medializationof tibial tubercle, DTT=distalizationof tibial tubercle, Y=yes, N=no. Patellar apprehension
was graded from 0 to ++: 0, no apprehension; +, discomfort on extreme lateral translation of the patellar in
extension, or true apprehension with voluntary quadriceps contraction on lateral translation in extension;
and ++, when the patient stops the clinician touching the patella.
Fig. 4: Kujala score at last follow-up according to pre-operative status. Two groups were constituted for
each of the 3 criteria analyzed (previous surgery, patellofemoral chondropathy, and patellofemoral
osteoarthritis according to the Iwano system [10]).











