
The Principles of an Ideal Patellofemoral Arthroplasty
295
Trochlear Component
It is not uncommon for patients with isolated
patellofemoral arthritis to have associated
abnormal
patellofemoral
biomechanics.
Trochlear dysplasia combinedwith an increased
tibial tuberosity-trochlear groove distance [22]
results in increased pressure on the lateral
aspect of the patellofemoral joint. This
predisposes the patella to sublux laterally. A
trochlear prosthesis with a steep, relatively
long prominent lateral facet would prevent the
patella subluxing, ensure contact in full
extension and engagement of the patella in
early knee flexion. If the lateral facet is too
prominent soft tissue impingement will occur,
therefore a balance must be found between
constraint and conformity.
In mid knee flexion, internal rotation of the
tibia will have reduced the Q angle and
consequently the lateral force, whilst the
posterior force is increased due to the angle
closing between the quadriceps and patellar
tendon in the sagittal plane. During this range
of movement the patellar component should be
stable; a trochlear component with a single
radius of curvature is sufficient to allow this
motion to take place effectively. The trochlear
component should fit flush over all aspects of
contact with the distal femur, avoiding the need
to place it in flexion or hyperextension, where
it will catch the patella or impinge onto the
anterior cruciate ligaments, respectively [23].
In deep knee flexion the patellar component
articulates with the articular surfaces of the
femoral condyles. The transition point from
prosthesis to articular cartilage must be even to
avoid any catching of the patella. All current
prostheses extend to the intercondylar notch
but not beyond. There is an assumption that the
articular cartilage adjacent to the prosthesis is
normal, however this is not true for all cases. A
wider distal endmay provide adequate coverage
for the more extensive wear patterns but
potentially at the expense of damage to the
menisci when the knee is extended, and
preventing the later addition of a unicom
partmental arthroplasty in the presence of
progression of tibiofemoral arthritis. This
means that the patellar component must be
compatible with the articular cartilage.
In the native knee the trochlea is asymmetrical.
The lateral articular facet is approximately
50% larger than the medial to accommodate
the higher load. It therefore seems logical that a
femoral component should mimic this
geometry, particularly when considering a
significant number of patients will have a
history of patellar instability with a tendency to
track laterally.
A
B
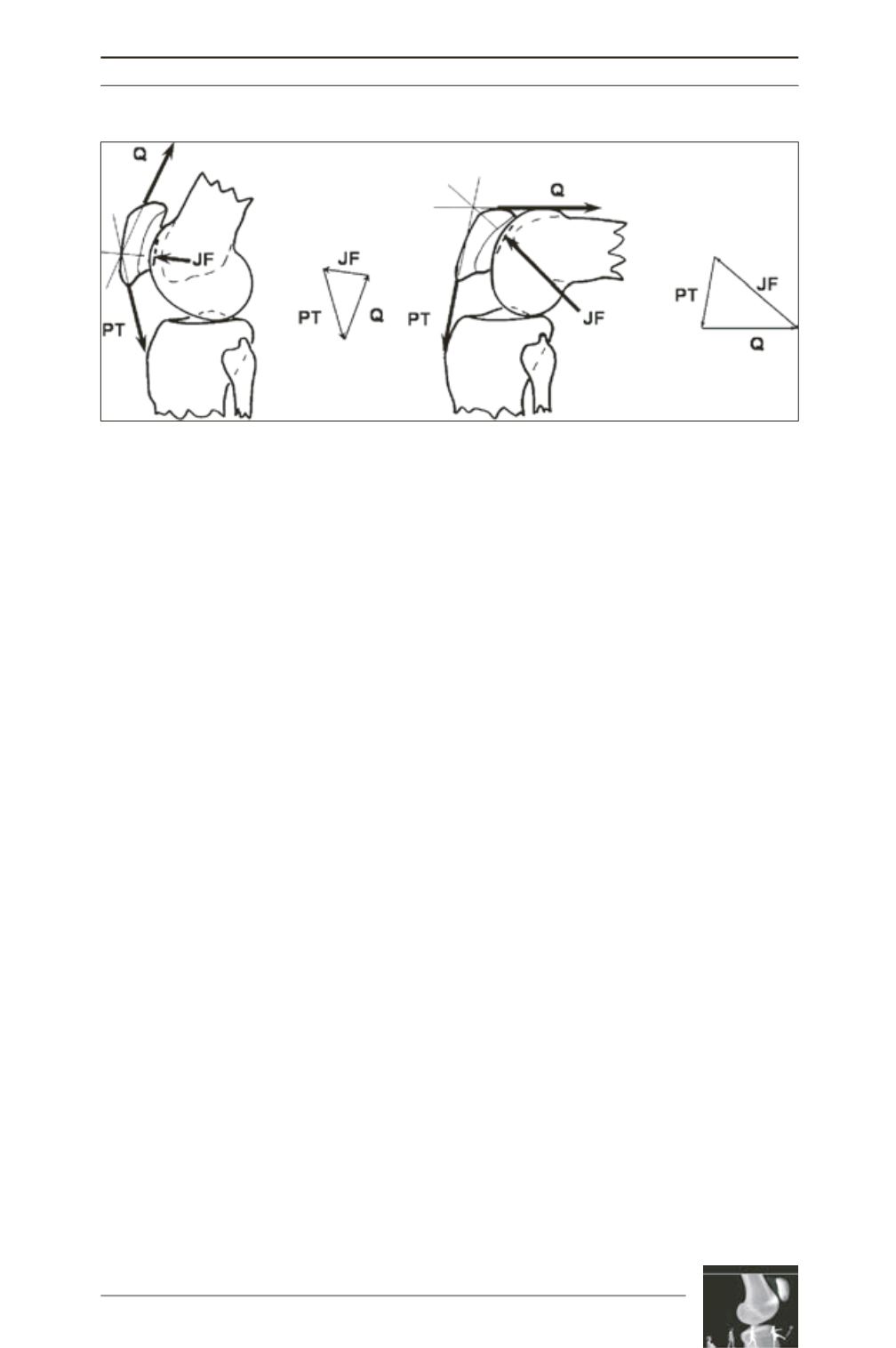
Fig. 6 : Forces acting on the patella in the sagittal plane. Quadriceps tension (Q), patellar tendon tension
(PT) and joint force (JF). The JF moves proximally across the patella as the knee flexes, rising significantly
with increase in knee flexion for the same PT.
Permission to use image granted by copyright owners Lippincott Williams & Wilkins. Amis AA, Senavongse W,
Darcy P. Biomechanics of patellofemoral joint prostheses. Clin Orthop 2005; 436: 20-9.











