different making knee arthroplasty a straight-
forward or a problematic endeavour. We sug-
gest to classify the pre-arthroplasty knee into
2 categories, dependant on valgus angle, range
of motion and patella position. In addition we
found that there is a third group of post HTO
knees that have very obvious problems that
require major modification of the operative
technique (Table 2).
If there is a patient with a small valgus over-
correction beneath 5°, with a range of motion
that does not differ from what’s to been seen
before primary total knee arthroplasty and a
correct position of the patella, knee replace-
ment will be straightforward and results will
not differ from what we expect in primary
knee arthroplasty without former HTO (fig. 1).
If a valgus angle has been produced by the
high tibial osteotomy that is higher than 5° a
juxtaarticular deformity has been created by
the first surgery. In these cases the knee itself
does not necessarily cause additional pro-
blems, but it is the iatrogenic deformity of the
tibia that has to be addressed. If in knee arthro-
plasty the advice given in some papers
(Krackow KA 1990) is followed, the bony
deformity of the tibia will be corrected within
the soft tissue envelope of the knee. That
would mean to add a soft tissue deformity to
the existing bony deformity. This is not our
procedure of choice but instead we suggest to
correct the bony deformity during knee arthro-
plasty (fig. 2). In class II deformities the sur-
geon has first – as always in TKA – to restore
direction and height of the joint line. He
should consider re-osteotomy of the tibia if
there is severe iatrogenic deformity. He should
consider osteotomy of the tibial tuberosity if
the position of the patella has been altered too
much. Soft tissue release is not a means to
address class II patients with severe bony
deformity.
Offset proximal tibia, severe bone loss or
pseudarthrosis of the tibia are all problems that
have to be specifically addressed in class
III patients. There might be a necessity to use
offset stems, modular long stems and even hin-
ged or custom made prosthesis (fig. 3).
14
es
JOURNÉES LYONNAISES DE CHIRURGIE DU GENOU
34
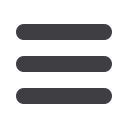
Author
Year
n Follow-up time
level
Katz MM
1987 21/21
3 yrs
81 %/100% good
III
Amendola A
1989 42/41
3 yrs
ROM
↓
III
Mont MA
1994 73/73
6 yrs
64%/81% good
III
Tokvig Larsen RS 1998 40/40
10 yrs
no difference (RSA)
III
Nizard RS
1998 63/63
4 yrs
more pain
III
Meding JB
2000 39/39
8 yrs
no difference
III
Karabatsos B
2002 20/20
5 yrs
poorer outcome, difficult
III
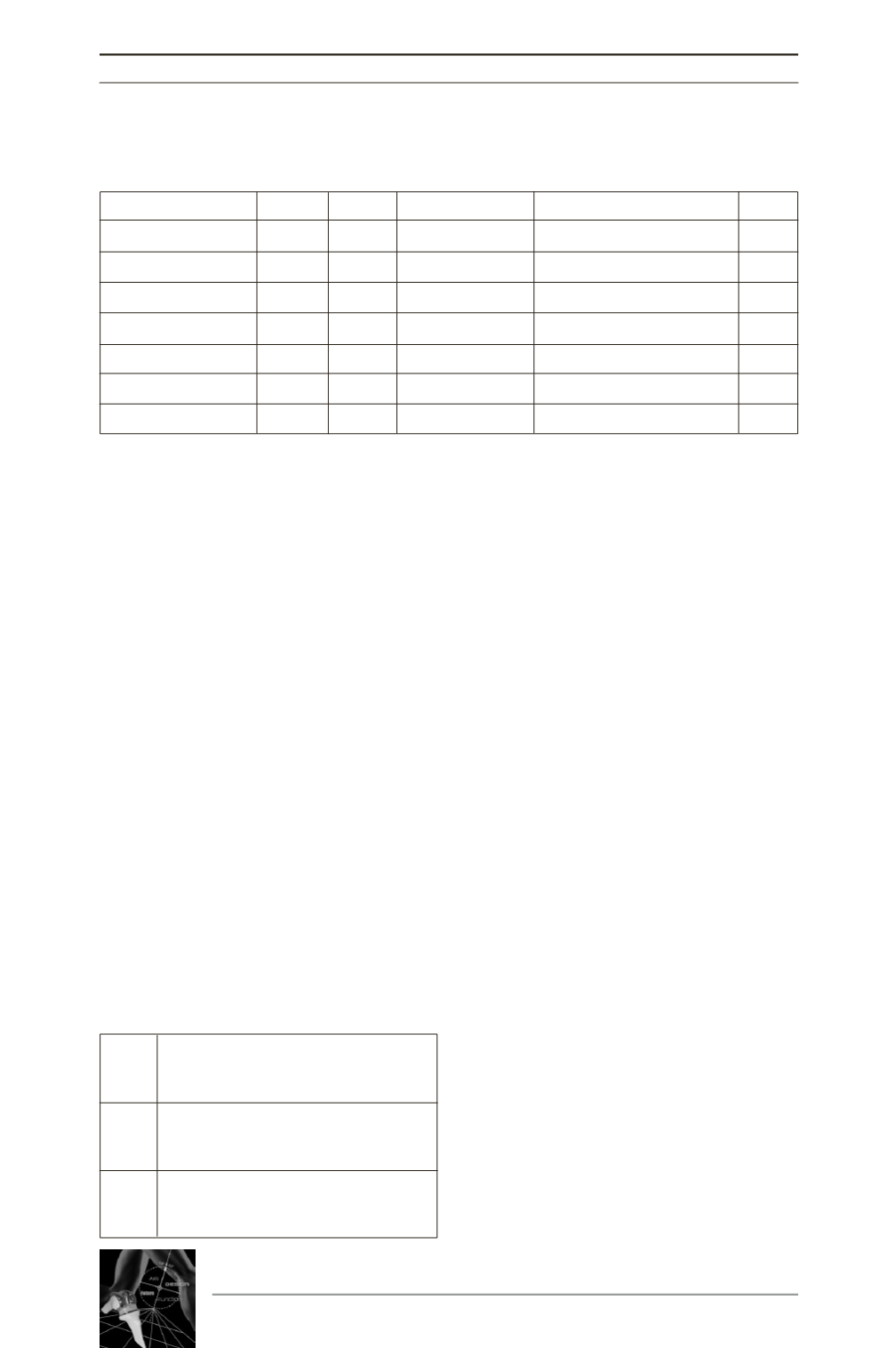
valgus angle < 5°
I
ROM > 0 – 5 – 120°
patella: position (nearly) normal
valgus angle > 5°
II
ROM < 0 – 5 – 120°
severe patella infera
offset proximal tibia
III
severe tibial bone loss
pseudarthrosis of tibia
Table 1 : Comparison of high tibial osteotomy and total knee arthroplasty
with primary total knee arthroplasty. The level of evidence is mentioned.
Table 2 : Suggested preoperative classifica-
tion of knees after high tibial osteotomy
before total knee arthroplasty. In class I
knee arthroplasty is not difficult, in class III
a complex procedure must be anticipated.











