
D. Dejour, P.G. Ntagiopoulos
176
than 80% of patients with patellar dislocation
the pathology is located in the middle (elevated
groove) and medial (hypoplastic facet) third
[46]. These patients would benefit from a
deepening trochleoplasty procedure [46].
Biedert
et al.
also studied trochlear dysplasia
with the use of convetional X-rays, axial CT
and MRI and presented another type of
trochlear dysplasia that could not be included
in the Dejour classification and where none of
the previously described radiological findings
existed: the “too short lateral articular trochlea”
[47]. They described the lateral condyle index
for assessing the length of the lateral trochlea
and defining the patients suffering from a short
trochlea who could be good candidate for
elevating trochleoplasty.
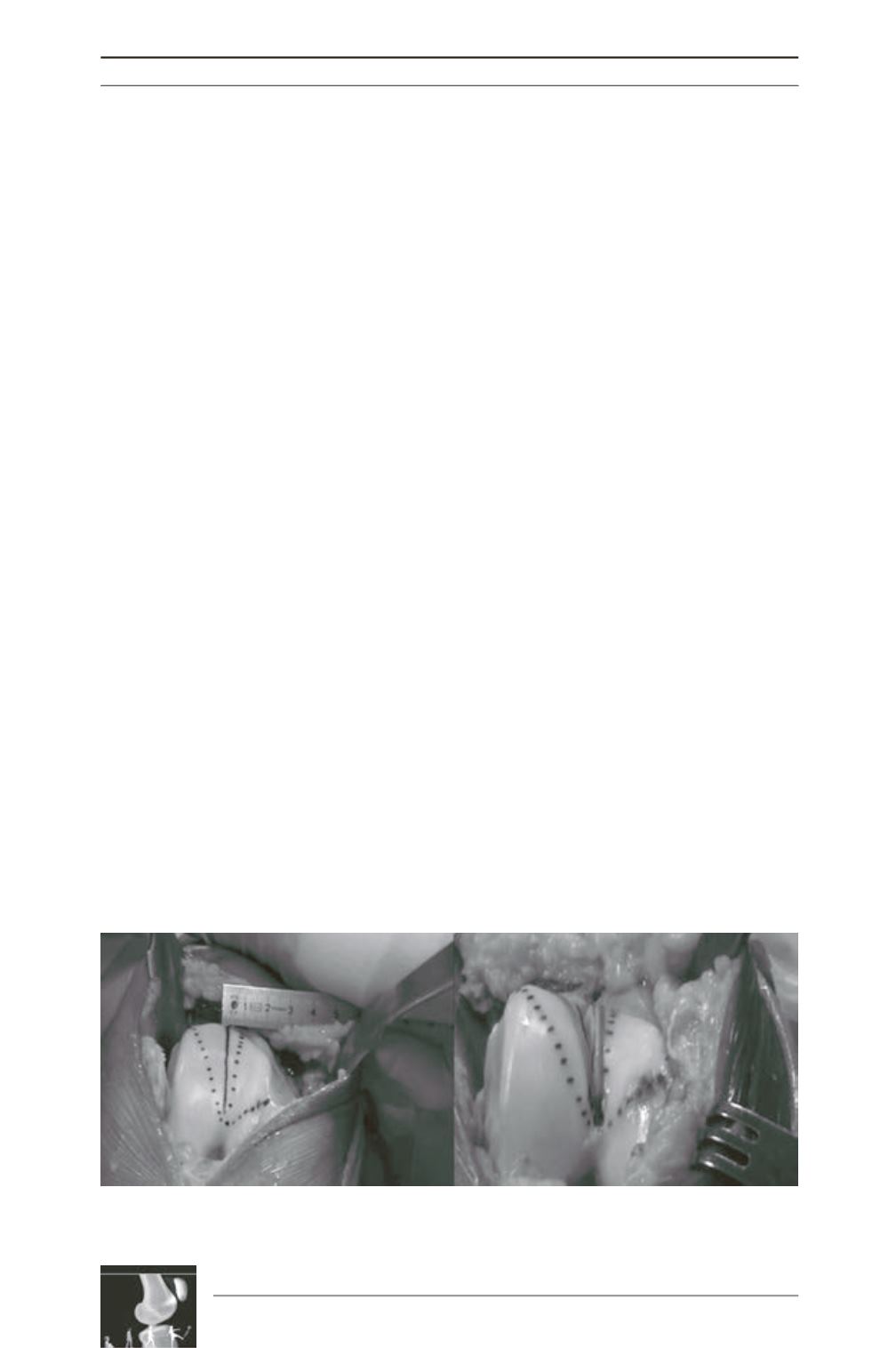
Finally, in 2010, D. Dejour presented the
modification of the “Lyon’s School” sulcus-
deepening trochleoplasty with the combination
of soft-tissue procedures for the treatment of
recurrent patellar dislocation in patients with
underlying high-grade trochlear dysplasia
(Type B and D) [48]. The rationale of this
surgical procedure is to restore the normal
anatomy and to re-shape the trochlea by
undermining the cancellous bone and deepening
the groove, to decrease the sulcus angle and
additionally, to perform a ‘proximal’ re-
alignement procedure by lateralizing the
trochlear groove (fig. 11) [48].
Although the origins of trochlear dysplasia are
scarce and reported up to two centuries ago, its
future study seems very promising. Currently,
there is ample interest on the diagnosis and
treatment of trochlear dysplasia. There is also
observer agreement on the classification of
trochlear dysplasia [44, 45]. Its contribution to
future degenerative joint disease is another
reason for the introduction of various techniques
to surgically correct it [2, 49]. Trochleoplasty
procedures aremore andmorewidely performed
as a primary or revision option in selected
patients with recurrent patellar dislocation and
underlying trochlear dysplasia. The recognition
of the importance of trochlear dysplasia in the
aetiology of patellar dislocation is growing and
has been embraced by surgeons in Europe but
also, in the United States [2, 9, 10], in the U.K.
[1, 24] and in Japan [50, 51]. There are
convincing data that there is a subgroup of
patients with recurrent patellar dislocation and
underlying high-grade trochlear dysplasia, in
which the
“benign neglect”
of the latter and the
application of traditional surgery is ill-fated [9,
35-37, 52, 53]. The sound biomechanical
evidence from the surgical treatment of
trochlear dysplasia [14] and the satisfactory
clinical results published by Von Knoch [35],
Verdonk [54], Donell [24], Blønd [38] and
Schöttle [55], Goutallier [36], Fucentese [56],
Thaunat [52], Beaufils [37], Dejour [57] and
others, confirm that trochlear dysplasia is a
distinctive pathology in the aetiology of patellar
dislocation, which must not be ignored or
under-diagnosed, and that its treatment should
be in the armamentarium of knee surgeons.
Fig. 11: The sulcus-deepening trochleoplasty removes cancellous bone and deepens the groove, decreases
the sulcus angle and performs a ‘proximal’ re-alignement procedure by lateralizing the trochlear groove.











