SURGICAL IMPLICATIONS
The ideal graft would have similar stiffness,
but be stronger, than the native MPFL. The
current tissue used to reconstruct the MPFL
is significantly stiffer than the native MPFL.
MPFL reconstruction with “stiff grafts” can
produce large increases in PFJ loading if
small errors in graft length and/or attach-
ment site are present. This will have its big-
gest consequence if the graft length is “too
short” for its arc of motion, and the length
change thru an arc of motion is restricted.
This will result in reduced ROM, increased
forces on the medial patella facet, or both.
Graft attachment points: more research is
needed. Some agreement that length change
pattern depends principally on the femoral
attachment point. The least change was with
a point more distal on the patella and more
proximal on the femur [16]. This was also
the site that had the longest length between
the 2 points. For one cadaver study [15], the
femoral attachment site was most sensitive
to position change, especially superior and
anterior. The ligament was “longest” at 60° of
flexion.
The graft length should allow the patella to
enter the trochlear from a lateralized posi-
tion, as dictated by normal PF kinematics,
and allow the slope of the lateral trochlear
wall and the lateral patella facet to engage its
trochlear position gradually.
Intra-operatively, one should adjust the
attachment sites to minimize the length
change with knee flexion. If lengthening
occurs in flexion, one can move the femoral
attachment site more distal. If lengthening
occurs in extension, one can move the femo-
ral attachment site more proximal.
We still lack any objective evidence for an
MPFL graft tensioning protocol. This must
be a compromise between over-constraint
causing medial patella pressure vs. slackness
which allows patella subluxation in early
flexion. It appears prudent to tension your
graft with the knee contained in the groove
at the ROM where your graft length in the
longest.
LATERAL-SIDED
LIGAMENTS
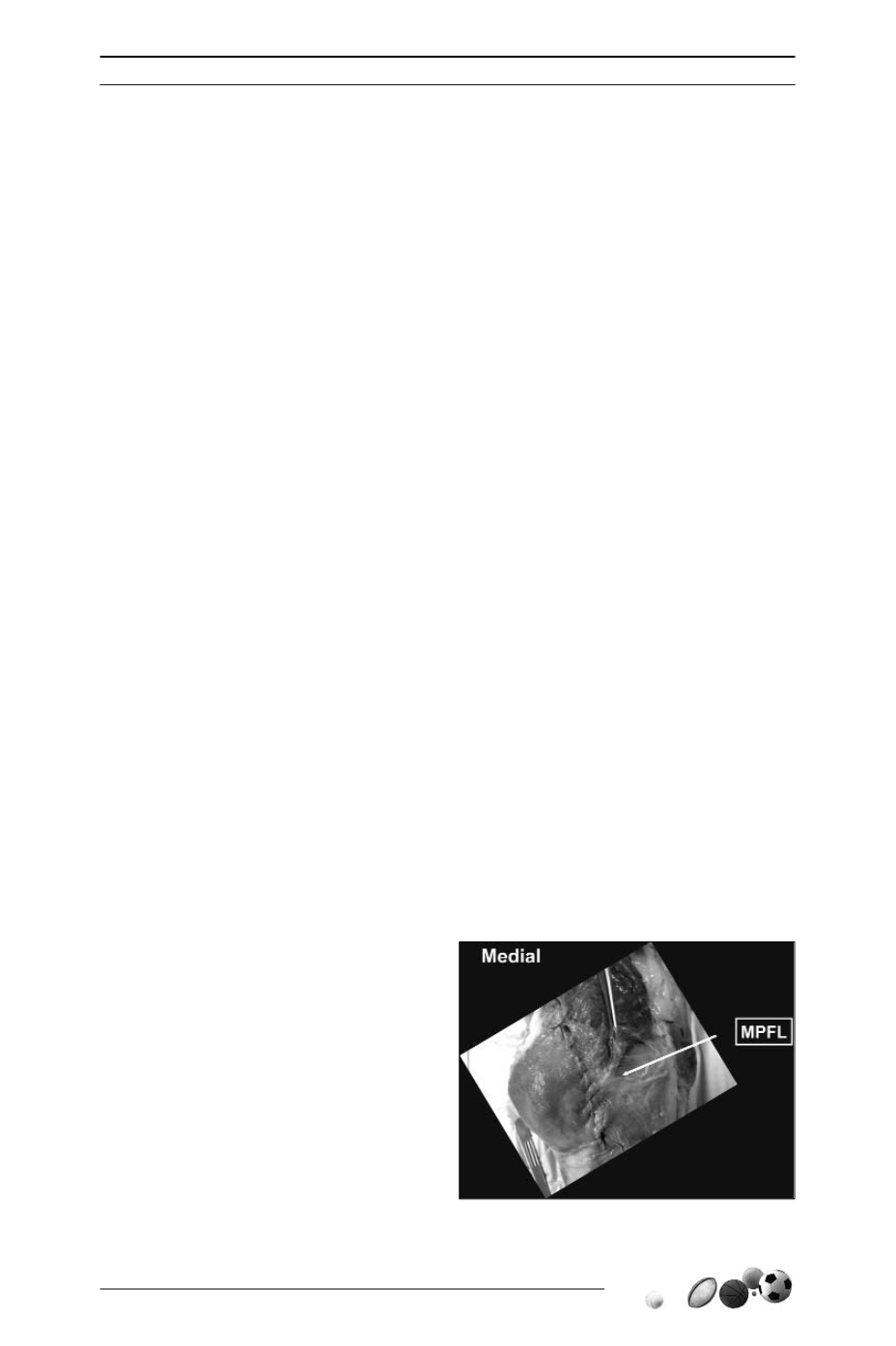
On the lateral side, the ligaments are a
confluence of fibers that extend from the
iliotibial track to the lateral border of the
patella. This is often referred to as superfi-
cial oblique retinaculum, but it contains the
lateral patellotibial ligament if one would try
to have symmetry with what we see on the
medial side.
However, the deeper layer has a transverse
retinaculum that does not insert onto the
femur, therefore “lateral patellofemoral liga-
ment” may be misnamed. There are signifi-
cant interdigitations between the superficial
oblique retinacular fibers and the deep
transverse retinacular fibers, often making
these two layers difficult to separate in spe-
cimens or patients (fig. 5).
The strength of the lateral retinacular fibers
individually is stronger than the medial side;
however, the layers typically combine with
specific interdigitations between them
making the two layers a much stronger
construct than its opposite medial side.
ANATOMY AND BIOMECHANICS OF PATELLOFEMORAL RESTRAINTS
39
Fig. 5











